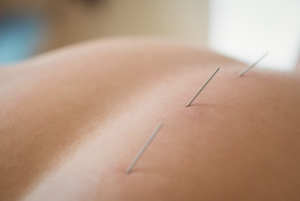
Image by wavebreakmedia_micro on Freepik
Trigger Point Dry Needling (TDN) is a therapeutic technique that has gained popularity for its potential to
relieve muscle pain and discomfort. Often compared to acupuncture, dry needling is a distinct approach to addressing muscle knots and trigger points in the body. In this blog, we’ll explore what trigger point dry needling is, how it differs from acupuncture, how it works, its potential pain level, and what to expect during and after the treatment.
What Is Trigger Point Dry Needling?
TDN is a therapeutic procedure that involves the insertion of fine, sterile needles into specific points in the muscles known as trigger points. Trigger points are tight knots of muscle fibers that can cause pain, limited range of motion, and discomfort. Consequently, this technique aims to release these knots, providing relief to the patient.
How Is Trigger Point Dry Needling Different from Acupuncture?
While both TDN and
acupuncture involve the use of needles, they are fundamentally different in terms of their principles, goals, and techniques.
1. Theory and Philosophy
Firstly, acupuncture is a traditional Chinese medicine practice. It based on the belief that the body has a network of energy channels, or meridians. Thus, the needles are used to balance the flow of energy (qi) within these channels.
On the other hand, TDN is rooted in Western medicine. Specifically, it targets muscle knots or trigger points believed to cause pain, muscle dysfunction, and other symptoms.
2. Needle Placement
Primarily, Acupuncture needles are often inserted along the meridians, which may be quite distant from the pain site.
On the contrary, TDN needles are inserted directly into the trigger points or tight muscle bands responsible for pain or discomfort.
3. Goals:
Overall, acupuncture aims to address a wide range of health issues, not just musculoskeletal problems.
Conversely, TDN primarily focuses on musculoskeletal issues, targeting trigger points and relieving muscle tension.
How Does it Work?

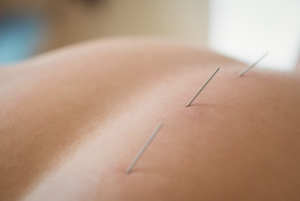
Image by tonodiaz on Freepik
TDN works through several mechanisms:
1. Stimulation and Relaxation: Essentially, the insertion of needles into trigger points stimulates the muscle fibers, causing them to twitch and relax. This helps reduce muscle tension and improve blood flow.
2. Pain Reduction: Additionally, this technique can trigger the release of endorphins, the body’s natural painkillers. Consequently, this may provide immediate pain relief.
3. Improved Range of Motion: Furthermore, by releasing tight muscle knots, TDN can enhance joint flexibility and range of motion. As a result, it is a valuable therapy for athletes and those with mobility issues.
Is it Painful?
The level of discomfort experienced during TDN can vary from person to person. Some individuals may feel minimal discomfort, while others may experience a temporary, sharp sensation when the needle is inserted into a trigger point. However, this discomfort is typically short-lived and subsides once the muscle relaxes. It’s important to communicate your comfort level with your therapist during the treatment to ensure adjustments can be made if necessary.
What to Expect During and After Treatment
During the Treatment:
- Initially, you will be asked to lie down, and the therapist will locate the trigger points through physical examination
- Next, sterile needles will be inserted into these points, and you may feel a mild discomfort or twitching sensation
- The therapist may gently manipulate the needles to stimulate the trigger points
- Overall, he entire session can last from a few minutes to around 30 minutes, depending on the number of trigger points being treated
After the Treatment:
- Some people experience immediate relief from pain and improved mobility
- You may also experience temporary soreness or bruising at the needle insertion sites. Usually, it resolves within a day or two
- Later, i’s recommended to stay hydrated, rest, and avoid strenuous activities on the day of treatment to allow your body to recover
In conclusion, Trigger Point Dry Needling is a Western-based therapeutic technique that focuses on addressing musculoskeletal issues by targeting trigger points in the muscles. While it involves the use of needles like acupuncture, the two practices differ significantly in their philosophies and goals. TDN can be an effective way to alleviate muscle pain and improve mobility, with the level of discomfort during treatment varying from person to person. If you’re considering TDN, consult with a
qualified physiotherapist to discuss your specific needs and expectations.