post-prostatectomy-incontinence
Post-prostatectomy-incontinence is a common problem after radical prostatectomy. Patients report that this is the symptom which most disrupts their quality of life. Up to 75 percent of men experience a short period of mild incontinence. This is particularly after removal of the catheter that was placed during surgery. Most patients regain total urinary control after radical prostatectomy. However, this can take up to a year to achieve. Apparently, a small percentage (2% to 4%) experience permanent incontinence. Following radical prostatectomy, men who experience post-prostatectomy-incontinence may express concerns about visible wetness, urine odor, and the type of clothing that can be comfortably worn.
Types of Urinary Incontinence
The two types of post-protatectomy incontinence following prostate surgery are:
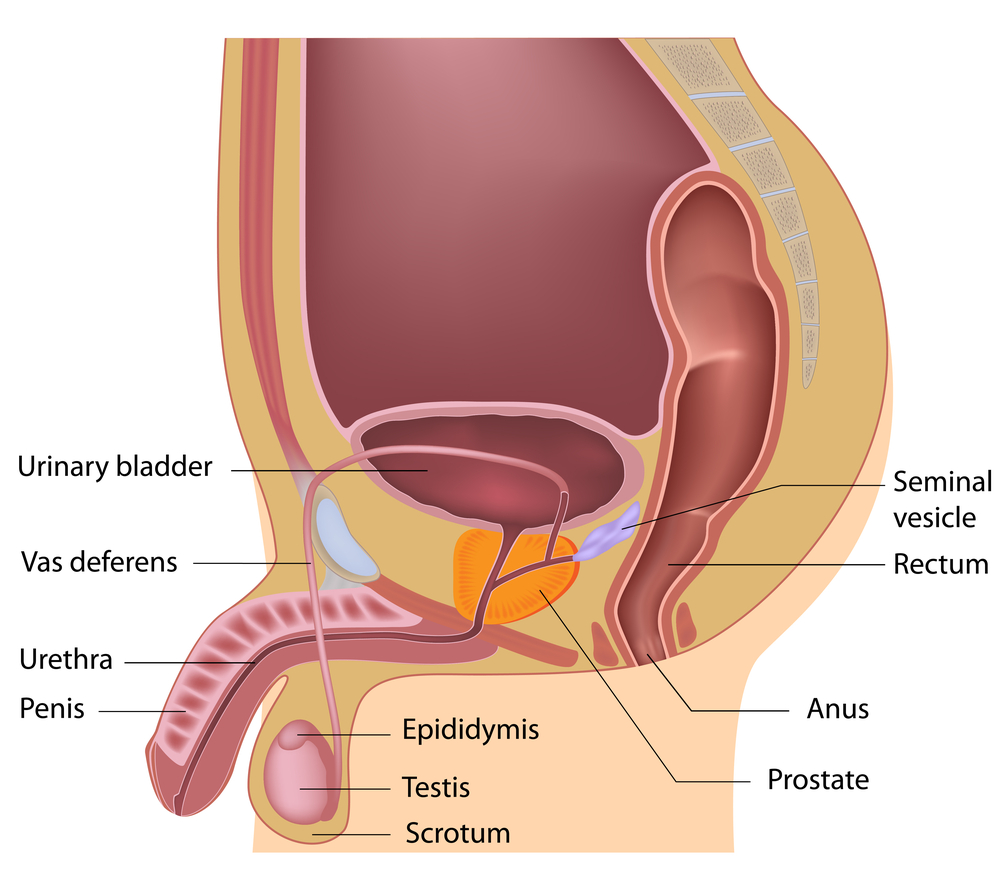
• Stress incontinence – Stress incontinence is the involuntary loss of urine that can occur during physical activity, like lifting a heavy object, or when you laugh or sneeze. These . activities put increased “stress” or pressure on the bladder.
• Urge incontinence – Urge incontinence is the sudden need to urinate due to bladder spasms or contractions.
What Can Be Done to Treat post-prostatectomy-incontinence after Prostate Cancer Treatment
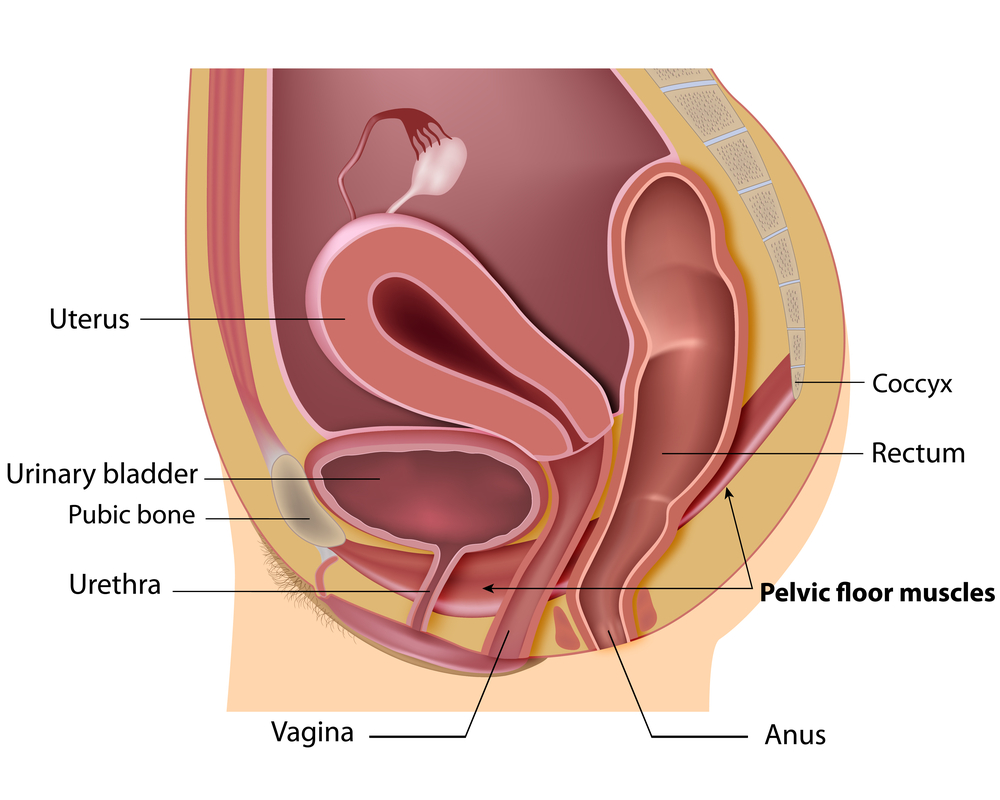
• Pelvic floor exercises: Kegel exercises strengthen the muscles when you squeeze them
• Stop urinating mid-stream. These exercises can be combined with biofeedback programs that help you train these muscles even better.
• Supportive care. This treatment includes behavioral modification. This includes drinking fewer fluids, avoiding caffeine, alcohol, or spicy foods, and not drinking before bedtime.
People are encouraged to urinate regularly and not wait until the last moment possible before doing so. In some people, losing weight may result in improved urinary control. Supportive care also involves changing any medications that interfere with incontinence.
• Neuromuscular electrical stimulation.
This treatment is used to retrain and strengthen weak urinary muscles and improve bladder control. With this treatment, a probe is inserted into the anus and a gentle current is passed through the probe at a level below the pain threshold.This causes a contraction. The patient squeezes the muscles when the current is on. After the contraction, the current is switched off.
As you can see, there are many things that can be done to treat post-prostatectomy-incontinence. PhysioNow has trained pelvic Health Physiotherapists ready to help you get started on regaining your life. It is hard to talk about these symptoms, and harder yet to find somebody who can help. Our therapists are sensitive and discreet. You will be treated in a quiet private room and your privacy will be fully respected. Get started today! Call today and ask for a pelvic health physiotherapy consultation at PhysioNow.

 can make a big impact on your bladder control.
can make a big impact on your bladder control.