Anatomy of the 1st CMC Joint
The 1st Carpo-meta-carpal (CMC) joint is more commonly referred to as the thumb joint. It is located at the base of the thumb between the carpal bones and the metacarpal bones. It is classified as a saddle joint, meaning it allows the thumb to move freely in many directions. As a result of this mobility, you can perform a wide variety of complicated tasks such as opening a jar, pinching an object, writing, and holding differently shape objects.
What is Thumb Arthritis?
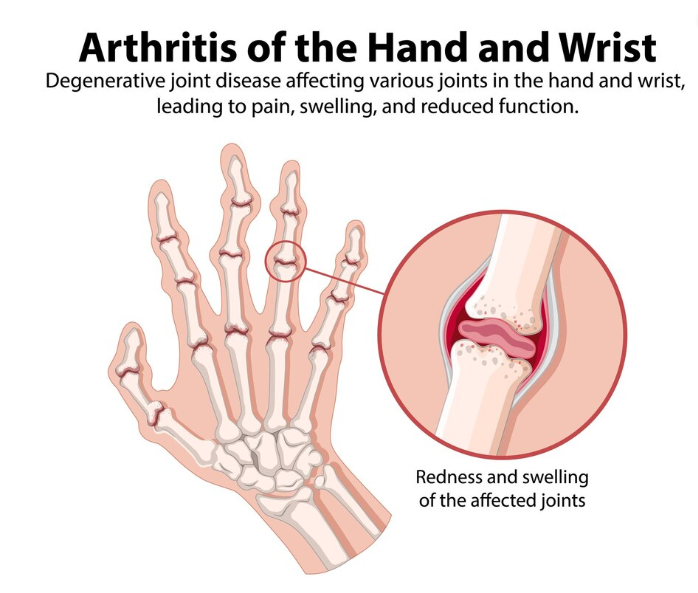
The bones that make up the CMC joint are covered in cartilage (tough but flexible tissue) which allows for smooth gliding in a healthy joint. With overuse and age, there eventual wear and tear on the cartilage which can result in the joint space narrowing and pain. Consequently, this increases friction within the space and can damage the joint tissues further. Osteoarthritis is the result of this overuse as the joint space narrows and more inflammation occurs as a result.
Symptoms of Thumb Arthritis
- Pain and tenderness at the base of the thumb
- Inflammation and redness around the base of thumb.
- Deformity in the shape of joint (dependent on severity)
- Pain with use
- Enlarged appearance of the CMC joint
- Reduction in strength of the joint
- Increase in pain while grasping (such as opening a jar) or pinching (turning a key)
Muscles of the Thumb
There are the group of muscles who covers the CMC joint and helps in different movements of the thumb.
Flexors group: writing and Pinching grip
Extensor + abductor group: wider grip like opening a jar
Role of Physiotherapy in Relieving Thumb Arthritis Pain

Physiotherapy plays a vital role in managing CMC arthritis by reducing pain and improving joint function and overall hand strength. Here are some key components of physiotherapy treatment for CMC arthritis:
-
Pain Management:
o Therapeutic Modalities: Physiotherapists use various modalities such as ice, heat, ultrasound, and electrical stimulation to reduce pain and inflammation.
o Manual Therapy: Gentle joint mobilizations and soft tissue techniques can help alleviate pain and improve joint mobility. -
Exercises to Improve Function:
o Range of Motion Exercises: Gentle stretching exercises help maintain and improve the range of motion in the thumb and hand.
o Strengthening Exercises: Targeted exercises to strengthen the muscles around the thumb and wrist can enhance stability and function. Examples include thumb abduction and opposition exercises using resistance bands or putty. -
Splinting and Support:
o Thumb Splints: Custom-made or prefabricated splints can provide support, reduce pain, and prevent further joint damage. Splints are often worn during activities that worsen symptoms. -
Activity Modification:
o Ergonomic Advice: Physiotherapists provide guidance on modifying daily activities to reduce stress on the CMC joint. This may include using adaptive devices or altering grip techniques.
o Joint Protection Strategies: Educating patients on techniques to protect the joint, such as avoiding repetitive gripping or pinching, can help manage symptoms and prevent further damage. -
Education and Self-Management:
o Patient Education: Understanding the condition and its management is crucial. Physiotherapists educate patients about self-care, treatment options, and the expected outcomes.
o Home Exercise Programs: Tailored home exercise programs empower patients to take an active role in their treatment, promoting long-term management and symptom relief.
Preventing Arthritis
While it may not be possible to completely prevent CMC arthritis, certain strategies can reduce the risk and delay its onset:
- Ergonomic Adjustments: Use tools and devices designed to reduce stress on the thumb joint during activities.
- Strengthening and Stretching: Regular exercises to maintain thumb and hand strength and flexibility.
- Activity Modification: Avoid repetitive stress on the thumb joint by varying activities and using proper techniques.
Need more help?
CMC arthritis can significantly impact hand function, but physiotherapy offers a range of effective treatments to manage symptoms and improve your quality of life. If you are experiencing symptoms of CMC arthritis or any other type, look for PhysioNow! We have many expert Physiotherapists that can support your recovery. Book with PhysioNow today for your first assessment and treatment.


