What is the Pelvic Floor?
 Pelvic floor muscles attach to the pelvis bone
Pelvic floor muscles attach to the pelvis bone
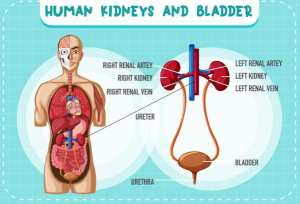
The pelvic floor is a group of muscles, ligaments, and connective tissues that span the bottom of the pelvis. Importantly, these structures support the pelvic organs, including the bladder, rectum, and in women, the uterus and vagina. The pelvic floor plays a crucial role in maintaining continence (control over bladder and bowel movements), supporting pelvic organs, and contributing to sexual function.
What are the most common signs and symptoms of pelvic floor
dysfunction?
There are several signs and symptoms for pelvic floor dysfunctions. They can be further subdivided into categories of urinary, bowel, sexual and pain-related issues.
Urinary Symptoms
1. Urinary Incontinence: Unintended leakage of urine, which can occur during activities like coughing, sneezing, or exercising (stress incontinence) or with a sudden, intense urge to urinate (urge incontinence).
2. Urinary Frequency and Urgency: Needing to urinate more often than usual or experiencing a strong, sudden need to urinate.
3. Incomplete Emptying: Feeling that the bladder isn’t completely empty after urination.
Bowel Symptoms
1. Fecal Incontinence: Involuntary leakage of stool or gas.
2. Constipation: Difficulty in passing stools, which might require straining.
3. Incomplete Evacuation: Feeling of not fully emptying the bowel after a bowel movement.
Sexual Symptoms
1. Painful Intercourse: Discomfort or pain during or after sexual intercourse.
Pain and Discomfort
1. Pelvic Pain: Persistent or recurrent pain in the lower abdomen, pelvic region, or genital area.
2. Lower Back Pain: Discomfort or pain in the lower back that might be related to pelvic floor dysfunction.
3. Pressure or Heaviness: A sensation of pressure, heaviness, or a bulge in the pelvic area, often related to pelvic organ prolapse.
What are the most common reasons for pelvic floor dysfunction?
Pelvic floor dysfunction (PFD) can result from a variety of causes, often related to factors that weaken or damage the pelvic floor muscles and connective tissues. Here are some of the most common reasons:
1. Pregnancy and Childbirth: Stretching, straining of pelvic floor muscles during pregnancy can lead to weakness and tearing of pelvic floor muscles.
2. Surgery: Surgeries such as hysterectomy, prostatectomy can weaken and affect your pelvic floor muscles.
3. Aging: Hormonal changes such as decreases in estrogen through general aging can also lead to weakening of pelvic floor muscles.
4. High Impact Chronic Strain: Frequent heavy lifting, chronic coughing, and bronchitis can also put excessive strain on pelvic floor muscles.
5. Neurological Condition: Conditions like diabetes induced neuropathy, multiple sclerosis, or spinal cord injuries can affect the nerves controlling the pelvic floor muscles.
6. Trauma and Injury: Injuries to the pelvic region due to physical trauma or stress can damage the muscles and nerves involved in pelvic floor function.
7. Lifestyle Factors: A sedentary lifestyle can lead to muscle weakening and tightening, leading to dysfunction in the pelvic floor.
Pelvic Physiotherapy
Pelvic floor physiotherapy is a specialized branch of physiotherapy involving internal and external assessment /treatment of pelvic floor muscles. These muscles are located between the hip bones, sacrum and support pelvic organs such as bladder, colon and uterus.
How physiotherapy can help with pelvic floor dysfunction?
Physiotherapy can be highly effective in treating pelvic floor dysfunction (PFD). Pelvic floor physiotherapists are specially trained to assess and treat issues related to the pelvic floor muscles, which can significantly improve symptoms and quality of life.
First, a comprehensive evaluation by a pelvic floor physiotherapist will include a detailed physical examination to identify the specific issues with your pelvic floor muscles. Then, based on the evaluation, the physiotherapist will develop a tailored treatment plan that addresses your specific symptoms and underlying causes. For example, this may include muscle re-education, bladder retraining, and training of the pelvic floor muscles.
Need help?
If you are experiencing pelvic pain or bowel or bladder dysfunction, look for PhysioNow. We have qualified pelvic floor physiotherapists that are ready to assist you with your issue. Book with PhysioNow today for your first assessment and treatment. With 9 clinics across the GTA including Burlington, Oakville, Mississauga and Etobicoke, we can find a location that suits you!