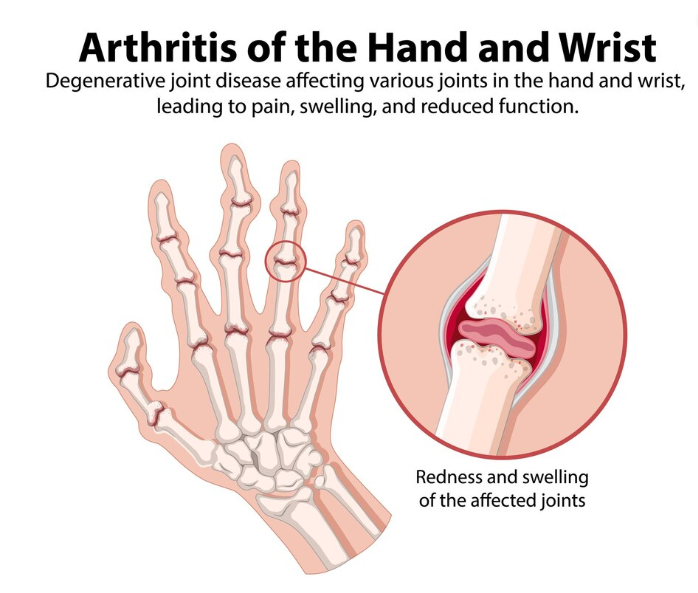
Rheumatoid arthritis (RA) is an inflammatory disorder that can affect multiple joints, usually on both sides simultaneously. In other words, if it affects your wrists, it would likely be both, not just one. RA is an autoimmune disorder. Essentially, a flare up is when your immune system starts to attack your own body’s tissues. Ultimately, it has systemic (body-wide) effects and can damage your skin, lungs, heart and blood vessels in some cases. RA mainly damages the lining of your joints causing large amounts of pain and swelling that can eventually result in joint line erosion and deformities. In most cases, the damage is permanent and leads to a decreased quality of life and increased disability.
What increases the risk of developing Rheumatoid Arthritis?
The ultimate cause of rheumatoid arthritis is unknown, but what we do know is certain things increase the risk of development. This includes:
- Family history
- Smoking
- Obesity
- Environmental or external factors (exposure to pollutants, stress, infection etc)
- Sex: Women develop RA more often than men
What are the signs and symptoms of Rheumatoid Arthritis?
The symptoms depend on the current stage the condition is in, and it cycles between two stages:
- Relapsing: Also known as a flare up, symptoms appear and are more intense
- Remitting: Symptoms including pain will decrease or are absent, but structural deformities will persist
During a relapse/flare up, symptoms include:
- Pain in the joints, usually 4 or more joints at a time
- Warmth and redness around the affected joints
- Swelling
- Tender to the touch
- Morning stiffness
- Fever
- Fatigue
In the early stage of RA, the small joints of the body like the fingers or toes are more affected. As the disease progresses, the larger joints become involved like the wrists, knees, ankles, elbows and hips.
How is rheumatoid arthritis diagnosed?
Primarily, RA is identified through a combination of a physical exam, analysis of your health history, x-rays and other imaging tests, and blood work looking for markers that may indicate the presence of the disease.
Physiotherapy Management of Rheumatoid Arthritis
- Education about the condition and the key role of interprofessional and collaborative care in the management of RA:

Your Physiotherapist can help you understand the condition, identify early signs and advise you on how to proceed or where to seek help. For example, they may help connect you to a medical doctor and a rheumatologist (professional that specializes in the care of inflammatory conditions) for specific management of RA. Additionally, these specialty clinics may provide additional resources for the management of the condition.
2. Activity modification
During a flare up, strenuous activity should be avoided and rest becomes the priority. This may include things like lifting, climbing stairs, and even walking can put excessive pressure on the joints. To help, your Physiotherapist may give you strategies to help you manage fatigue, conserve your energy, and prescribe you with a gait aid or other adaptive devices. For example, using a walker or cane to offload the lower body, or installing railings or raised toilet seats.
3. Therapeutic exercise
During periods of remission, therapeutic exercises will be used to maintain normal muscle strength and prevent deterioration. The duration, severity, and types of exercise will be determined after a thorough assessment. Your Physiotherapist will uniquely adapt the exercises to an appropriate level for your condition. Overall, these exercises could include range of motion and stretching, aerobic conditioning, and strengthening.
4. Manual therapy
Manual therapies like soft tissue release, gentle joint mobilizations, and other massage techniques are useful for relieving pain and swelling and improving flexibility. It is also beneficial for promoting a general feeling of well being and increasing mood, which is often affected in this condition. Thus, it is an important part of the management of RA.
Where can I find help?
If you are experiencing difficulties with RA or any kind of joint pain, look for PhysioNow! We have many expert Registered Massage Therapists and Physiotherapists that can help you with your recovery today. With 10 clinics across the GTA from Burlington, Oakville, Mississauga, and Etobicoke, our highly accessible locations are ready to serve you! Book with PhysioNow today for your first assessment and treatment!