Pregnancy is an exciting journey, but it can be nerve wracking as well when it comes with many changes in the body. Unfortunately, these changes usually have side effects which include nausea, discomfort, fatigue, soreness, and pain. This alongside a disruption in your normal lifestyle can be very hard to adapt to. Many will wonder whether there is anything that can help. As a result, a common question that comes up with expecting mothers is it safe to do exercises and if yes, what can I do?
The good news is that, with the right guidance, doing exercises not only safe but also beneficial for mom and baby! Physiotherapists are experts that specialize in movements and body mechanics. Thus, this means they can recommend safe, effective, and individualized exercise programs to help through your pregnancy.
Why does exercise matter during pregnancy?
Fortunately, lots of research has gone into this topic, and the science supports it. The American College of Gynecologists and Obstetricians actually recommends 150 minutes of moderate aerobic exercise each week. In fact, if you were already active before the pregnancy, it is recommended to continue at that same level as long as your or comfortable. The possible benefits of staying active during pregnancy include:
- Easing back pain
- Decreases risk of pregnancy complications like gestational diabetes, preeclampsia and cesarean births
- Improving circulation, can be beneficial in the case of swelling
- Helping your body to prepare for labour with better endurance and flexibility
- Supports mental well-being by reducing stress and improving sleep
- Help with the recovery after delivery and return to your normal weight
However, it is important to understand that not all exercises are safe. For example, extreme and contact sports or hot yoga are not recommended due to risks of trauma and overheating respectively. Your physiotherapist can help you to create a program that is personalized for you, depending the trimester, and previous physical fitness, and medical history.
What do I need to know before exercising during pregnancy?
There are still some risks with exercising, but the benefits far outweigh the risk as long as we follow some safety tips.
- Initially, get a clearance from your ob-gyn or doctor to continue exercises
- Avoid overheating and dehydration
- Listen to your body and stop if you feel dizzy, breathless, or experience pain
- You may benefit from belly belts and a supportive sports bra for comfort
What are some safe exercises recommended by physiotherapists?
1. Walking or biking
Walking and biking are one of the safest and most accessible exercises during pregnancy. It helps to keep your body active without putting too much stress on your joints.
2. Prenatal yoga and stretching
Gentle yoga can help to reduce pain in your back and hip area which is very common in pregnancy. It can also help with flexibility, posture correction and with stiffness. Experienced physiotherapists can teach appropriate poses and stretches, and modifications as needed.
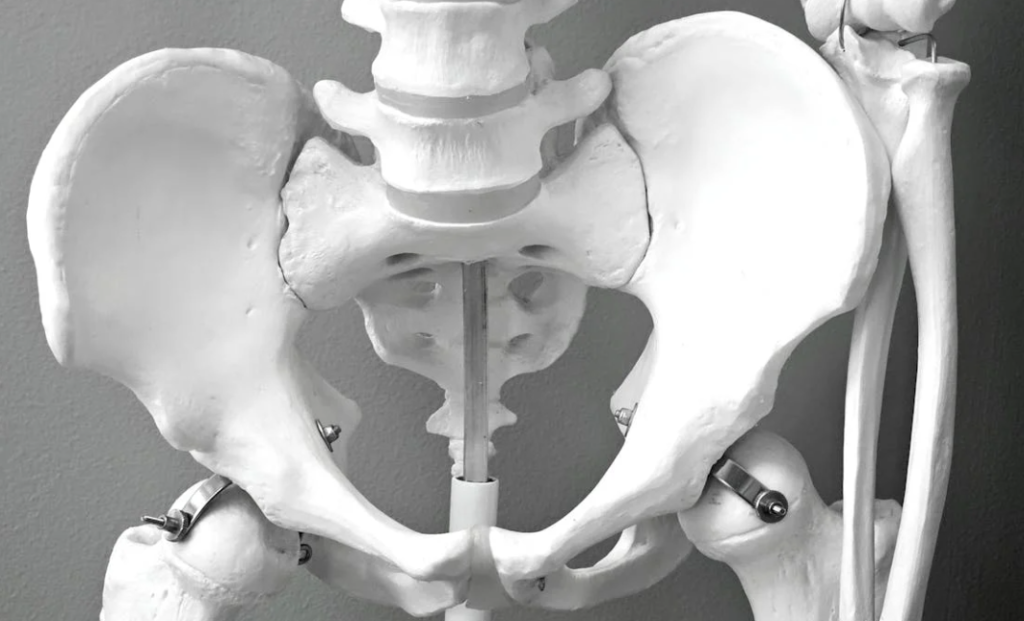
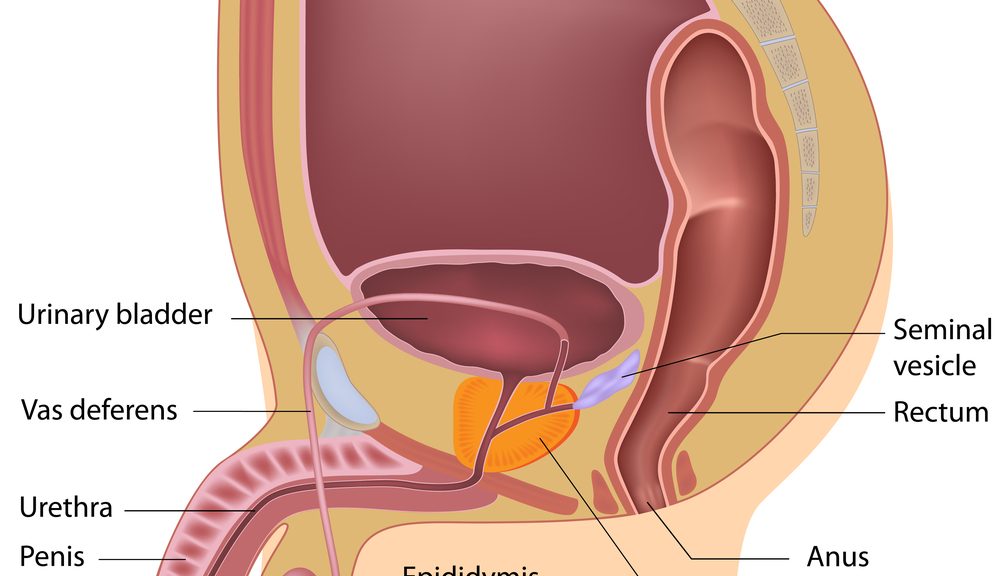
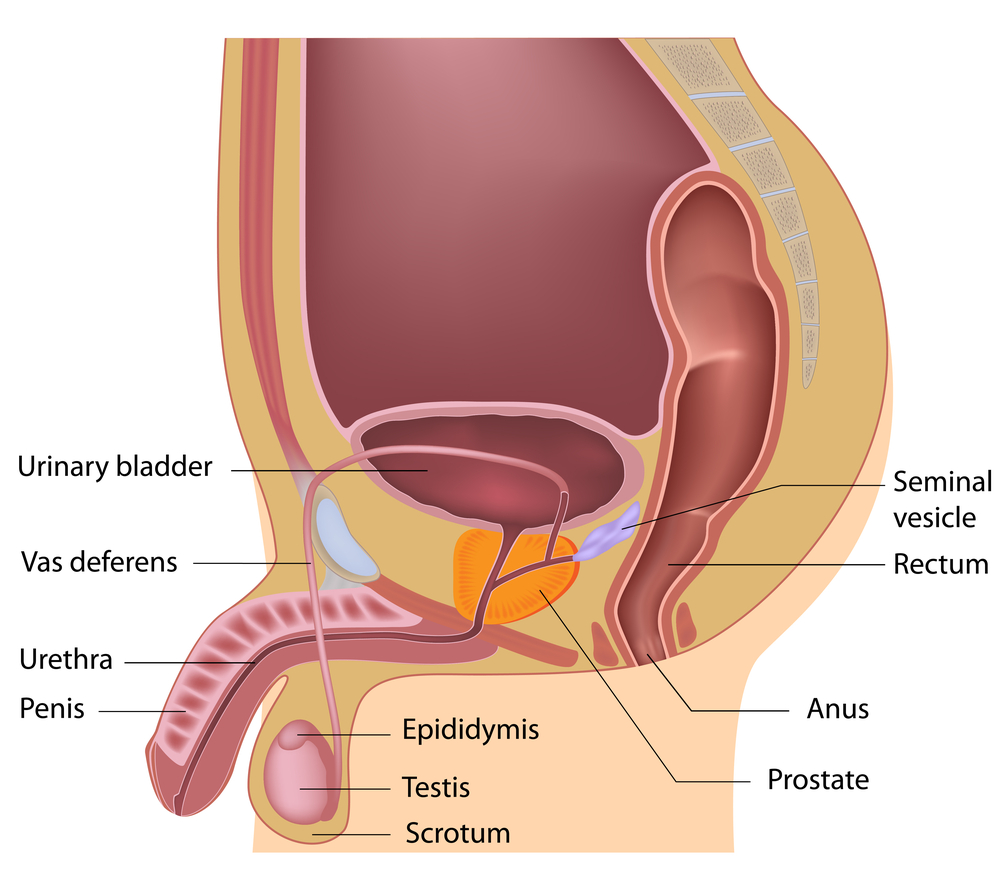
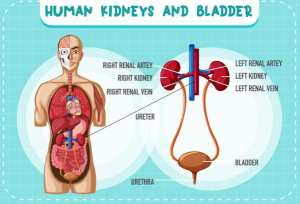
3. Pelvic floor exercises
It is crucial during pregnancy to strengthening the pelvic floor muscles. These exercises support the pelvic structures, and help to reduce the chances of getting incontinence (inability to control urination) during and after pregnancy. A trained pelvic health physiotherapist can teach you how to activate the right muscles.
4. Core and stability training
Safe core exercises, such as pelvic tilts or modified planks, strengthen the abdominal and back muscles. This helps support the shifting posture of the body to accommodate the growing belly.
5. Swimming or water aerobics
Performing exercises in water can help swelling and helps to take the extra weight off the body for a bit. The water supports your weight while also providing great resistance for a full body workout.
6. Light resistance training
It’s safe to use weights or resistance bands to maintain muscle tone and to prepare the body for the physical demands of childbirth and postpartum care. A supervised exercise program can help you to maintain controlled movements, good form, and proper breathing.
What are exercises to avoid during pregnancy?
• Standing for long period of time in same position
• Exercises lying flat on your back for long periods in your second and third trimester as it can restrict blood circulation to fetus
• Heavy weightlifting or straining movements
• Activities where there is a risk of fall or contact ex. skiing, basketball, soccer
What is the role of a physiotherapist in exercising during pregnancy?

Every pregnancy is different, a physiotherapist can:
• Help to assess your posture, movement, and areas of weakness
•Teach safe exercises program which is safe for you and adjust them based on your trimester
•Help manage common pregnancy complications like back and pelvic pain, sciatica pain
•Provide education on what to expect and how to set yourself up for success before, during, and after pregnancy
Ready to get started?
If you or anyone you know is pregnant and confused with what to do or how to start exercises safely look for PhysioNow! We have 10 clinics across the GTA to support you from Burlington, Oakville, Mississauga to Etobicoke. We offer private treatment rooms, free and accessible parking, and extended hours including evenings and weekends for your convenience. Book an assessment and treatment with our experienced physiotherapy team today to receive a safe, personalized plan that supports both you and your baby!