When we hear the word “falls,” we often connect it with an older generation. While it is true that with increasing age the risk of falls also rises, it is a risk that can affect a person from any age group. Starting from childhood to young adulthood, from an athletic to or weekend warrior population.
At our clinic, we consider balance training an integral part of every treatment, whether it is geared towards performance improvement, prevention, or rehabilitation. No matter which age or activity level group you belong to, good balance is important to injury prevention, stability, and confidence in how you move.
Why should I care about balance?
Your ability to maintain control while you are still or while you are in motion is called balance. There are two types of it:
- Static Balance
- Dynamic Balance
Static balance refers to times when your body is still, and trying to maintain a position. Common examples include yoga poses, standing on one leg, standing with your eyes closed and more.
Dynamic balance includes when your body is moving or being acted on by an external force. For example, you’re using dynamic balance when you’re walking, playing a sport, or riding a bus. They can range from easier tasks like walking on flat ground, to more difficult such as single leg squats on a bosu ball. A well-trained dynamic balance system is especially important during for preventing injuries during sports and daily life.
Which systems are in charge of balance?
There are many systems which gets involved and work closely together while maintaining balance. These include the following structures/systems:
- Connection between your muscles and joints
- Eyes (visual input)
- Inner ear (vestibular system)
- Nervous system (communicating with other parts of your body, processing all the sensory information, and proprioception, or your body’s ability to sense where it is in space)
Unfortunately, if there is any disturbance with one or more of them it can severely affect your balance. For example injuries to your joints, a traumatic brain injury such as a concussion, an ear infection, or other vestibular disorders can all affect your balance.
Who’s at risk (besides seniors)?
Although anyone can experience balance problems, you may be more vulnerable if you:
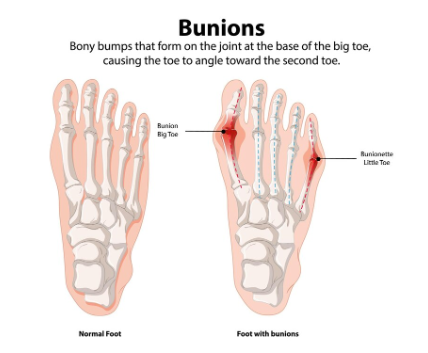
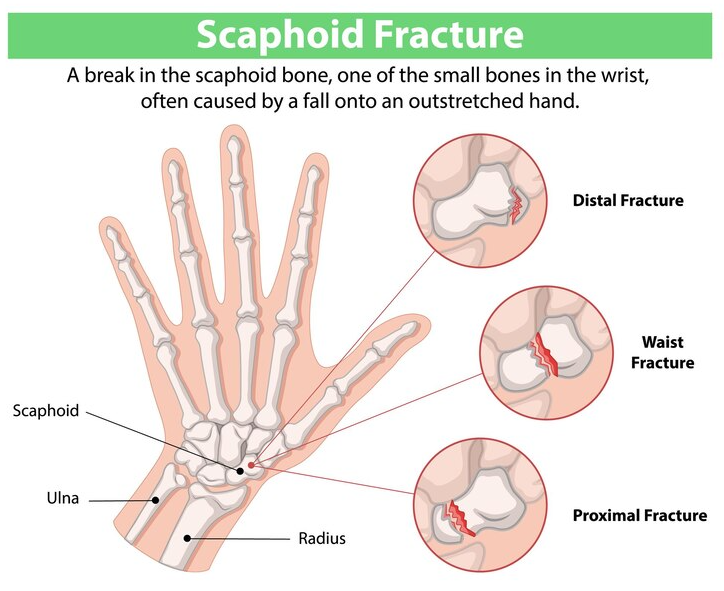
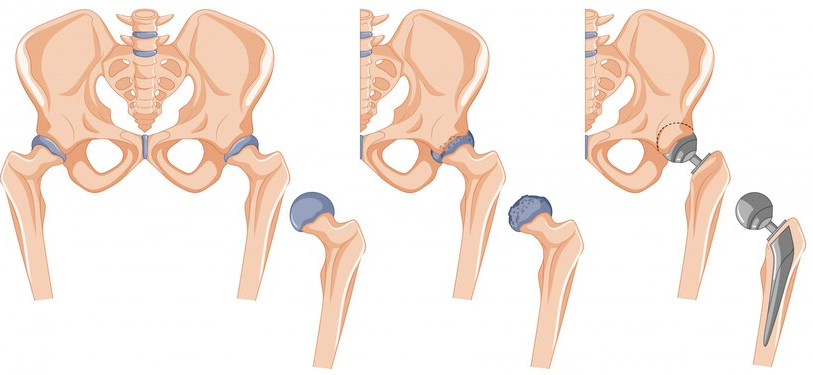
- Recently had a sprain or surgery, especially in the lower limb
- Have or have had in the past a traumatic brain injury (ex. concussion)
- Play competitive sports which required fast direction changes for example baseball, soccer, rugby etc.
- Have a history of vertigo or dizziness
- Have decreased or altered sensation in your lower limbs (ex. common in people with diabetes
- Have severe or uncompensated vision issues
How do I know if I my balance needs work?
- You find yourself tripping often
- You constantly reach towards and grasp walls or pieces of furniture
- You are scared or avoid uneven surfaces, curbs, or stairs without extra support
- You lose your balance or feel dizziness while standing with closed eyes or in the dark
- You feel “off while unsteady while walking or turning
There are also a few types of objective tests we usually perform to check your balance. It’s always advisable to perform under the guidance of professional or under supervision.
- Single Leg Stance Test: In this, we make person to stand on one leg for 30 sec or as long as they are able to. They are observed for any difficulties with balance or safety.
- Tandem Walk: We make them walk heel-to-toe in a straight line and observe for difficulties with balance
- Eyes-Closed Balance: In this one, we will have the patient stand with their feet close together and with the eyes open. We measure the time they can stand and then we repeat and compare it to their time with closed eyes
How can physiotherapy help improve my balance?
Your Physical Therapist can help you get started by assessing the cause of your balance issue. Whether it’s from a previous injury, a vestibular disorder, post-surgery or more, each will have a different type of treatment. Your physiotherapist will use the assessment to identify your specific impairments and create a personalized Fall Prevention Plan. It will also be targeted towards your goals, whether its to get back to your day to day activities, a specific sport, or just to feel more confident in yourself. They will use a combination of strengthening and coordination exercises, Vestibular Treatment if necessary, and offer education and lifestyle advice to prevent injuries in future,
Tips to reduce fall risk at home!
- Practice standing on one leg with some stable surface around and add it in to your day-to-day activities like cooking or brushing your teeth
- Focusing on strengthening the muscles of your lower extremity and core
- Try to walk on different surfaces to get practice and sensory feedback
- Wear well-fitted and properly cushioned shoes
- Try to keep your rooms clean and cluttered free
- Try to use bright lights around the house and staircases to avoid falls
Looking for more help?
Look for PhysioNow today! If you are having any issue with your balance, connect with our team of experienced therapists. You will be surprised with the results of how small steps can quickly give you the confidence to move better! With 10 spacious clinics across the GTA from Burlington, Oakville, Mississauga to Etobicoke, we are ready to get you started. Book with PhysioNow today for your first assessment and treatment!