What is sciatica?
Sciatica is a term that gets used quite frequently in the physiotherapy world. It refers to pain, tingling and/or numbness that goes down the back, hip or entire leg. It can happen to both younger and older adults for many reasons. For some, it starts after a traumatic event like a slip and fall or after a motor vehicle accident. For others, however, it starts gradually then suddenly increases in intensity over time. Despite the exact cause, sciatica can be a very difficult condition to go through.
Where does the term sciatica come from?
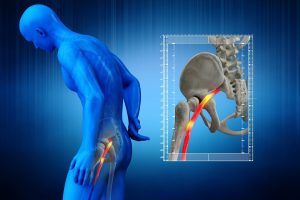
The term sciatica refers to irritation of the sciatic nerve, which is the largest nerve in our body. This nerve has its roots at the lower levels of the lumbar spine and runs through the gluteal area down the back of the thigh. Around the the knee, the sciatic nerve splits up into several smaller nerves that run down to supply the muscles of the lower leg, ankle and foot. The pathway of the sciatic nerve is important because the symptoms of sciatica can travel anywhere along the nerve.
What are the most common signs and symptoms of sciatica?
Symptoms of sciatica can affect one or both legs. The most signs and symptoms of sciatica include:
- Pain in the low back, hips and leg(s)
- Loss of range of motion through the low back
- Pins and needles going down the leg(s)
- Numbness or loss of sensation down the leg(s)
- Weakness in different muscles in the leg(s)
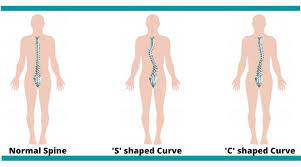
- Shifted postural alignment
- Some people are bent sideways
- Other people are stuck in a bent forward position
How can sciatica affect your day to day activities?
The exact ways that sciatica can affect a person will vary from person to person. However, most people with sciatica do have similarities in what they experience. For example:
- Pain with sitting for long periods of time
- For example, while working or driving
- Difficulty with getting up from prolonged sitting
- Cannot tolerate standing in one spot for prolonged periods of time
- Pain or inability to bend forward
- For instance such picking something off the floor or putting on socks
- Disturbed sleep
- It may be difficult to find a comfortable position
- Changing positions during sleep may cause intense pain
- Inability to walk for long periods of time
How severe can the symptoms get?
Sciatica can be very debilitating when it is in the acute stage. Pain can be quite sharp and severe, limiting mobility and function completely. A lot of patients at this stage will rate their pain intensity at a 9 or 10 out of 10. Any position or movement may be pain producing and anything they try, including over the counter medication, may not help with the intensity of pain. A lot of patients feel very helpless and scared at this stage. The sudden onset of intense pain makes these patients wonder if there is something seriously wrong. A lot of people go to the emergency room because the pain is so severe. At the hospital, the standard procedure will be to rule out anything potentially serious first.
What are some of the more serious causes of severe low back pain?
- Fracture
- History of significant trauma
- If there is osteoporosis present, then minor traumas are risk factors
- Loss of function with all movements making pain worse
- Cancer
- Risk factors for cancer can include:
- 55 years of age or older
- Previous history of cancer
- Unexplained weight loss
- Increasing pain that is constant and not relieved by rest
- Infection
- Signs and symptoms of an infection include:
- Fever
- Malaise
- Constant pain
- All movements make pain worse
- Cauda Equina Syndrome
- Severe low back pain
- Pain, numbness or weakness in one or both legs
- Saddle anesthesia
- Loss of or altered sensations in your legs, buttocks, inner thighs, backs of your legs, or feet
- Sudden sexual dysfunction
- Sudden changes in bowel or bladder functions
- Difficulty with relieving yourself or difficulty with holding it in
Any of the above-mentioned conditions would require emergency medical treatment, which the hospital would provide. However, for most patients, their sciatica is not from anything potentially serious. Most incidences of sciatica are mechanical in nature and can be treated. Once the hospital has ruled out anything serious, they will likely prescribe medication for pain management and provide a referral for physiotherapy.
What is causing the sciatica symptoms?
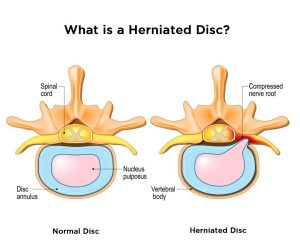
For most people, sciatica can be treated with conservative treatment such as physiotherapy. The important thing about treating sciatica is to determine the correct source of the pain and address those specific areas. With most sciatica patients, the pain is coming from pressure on one or more of the roots of the sciatic nerve. These nerve roots are found in the lower back. The pressure on the nerve affects the proper function of the nerve and causes the symptoms going down the leg.
Are the symptoms permanent?
It is important to note that, in most cases, the tingling, numbness and weakness in the leg is not something that will be permanent. A good analogy for this process is like when someone is stepping on a water hose. The pressure from the foot stops the water from passing through the hose. However, once that foot comes off the hose, the water will flow through without any issues. Similarly, the symptoms along the leg will get better once the pressure is removed off the nerve. Specifically with sciatica, the pressure on the nerve is usually caused by intervertebral discs or bony changes in the area.
Can physiotherapy help with sciatica?
Physiotherapy can definitely help with sciatica! An experienced physiotherapist will be able to perform a thorough assessment that will determine the potential cause of the sciatica. Once this cause is understood, the physiotherapist will be able to provide the most appropriate treatment to take the pressure off the nerve.
What does physiotherapy treatment involve?
Physiotherapy treatment for sciatica usually consists of multiple components. Lots of research out there has shown that passive treatments such as heat, ice, and electrical modalities, like IFC and ultrasound, do not provide long term solutions. However, these types of modalities may be useful in the acute phase to help with the management of pain. They can be combined with other treatments, including exercises and manual therapy, as part of the overall treatment plan for sciatica. However, on their own, they are unlikely to make any significant and long-lasting changes.
More importantly, there has to be an evaluation of what positions and/or movements are pain producing and which are pain relieving. A physiotherapist who has lots of experience working with low back issues will be able to help make this discovery. The results of the movement assessment will allow for the prescription of the appropriate exercises to help take the pressure off the nerve roots. The movement assessment will also help to determine which manual treatment techniques are most appropriate for the patient.
For example, if the patient feels less leg pain when they arch their back backwards, then that means their nerve is less irritated with that movement. Their treatment plan will therefore include exercises that involve various forms of back extensions that continue to improve their symptoms. The manual treatment provided will also help to improve this movement pattern and increase flexibility in general.
How long does it take for sciatica symptoms to improve?
As the pressure on the sciatic nerve improves, the pain will move upward towards the low back in a process called centralization. These changes may happen quickly for some patients. However, with more complex cases, it usually takes several weeks to ease the pain and regain function. Any exercises that are producing centralizing symptoms are going to be beneficial in creating lasting changes. Once the leg pain is better, strengthening for the back, hips, and lower limbs is important to prevent future episodes of sciatica.
In majority of cases, pain can be resolved completely, and the individual can return to their normal level of function. It is important that the physiotherapist provides education and a good home exercise program for the continued maintenance of the condition. Some patients will continue to avoid certain activities or movements because of their experience with sciatic pain. It is important for the physiotherapist to work with the patient to regain full function and confidence with their mobility.
If you have been experiencing sciatica, do not let the pain limit what you can do. Call and book your appointment with an experienced physiotherapist at PhysioNow today!