A pinched nerve, also known as a radiculopathy, is caused by pressure on a nerve as it exits the spinal cord, potentially causing pain, discomfort, weakness, and/or changes in sensation. Unfortunately, it can have quite detrimental effects on your daily life, hobbies, and ability to work. In this blog, we will discuss the causes, symptoms, and most importantly, how physiotherapy can help you recover from this condition.
Why does it happen?

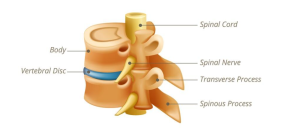
Model of the spine showing how the nerves (yellow) exit through spaces around the spinal column. The nerves may get pinched in these spaces.
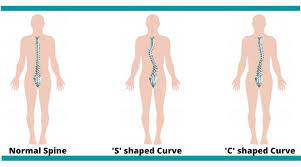
A pinched nerve occurs when there is compression or pressure applied to a nerve, disrupting its normal function. This compression can happen in various areas of the body but is most common at the spine of the lower back or neck. Common causes include repetitive movements, sudden increases in activity (ex. heavy lifting), poor posture, herniated discs, and degenerative changes in the back such as stenosis or bony spurs.
It is separate from the diagnosis known as a peripheral neuropathy that involves damage to the nerve. For example, a carpal tunnel syndrome. However, many of the symptoms between the two may overlap. In fact, a pinched nerve may turn into a neuropathy if left untreated for too long.
How do I know if I have a pinched nerve?
Primarily, nerve type pains have very specific symptoms. These usually include one, multiple, or all of the following:
- Pain: Sharp or dull pain that radiates along the nerve pathway. The pain is usually quite variable and may change quickly in intensity from one day to the next, or throughout the day.
- Sensation changes: This may be unusual sensations like pins and needles, losses of sensation, or even complete numbness in the affected areas.
- Muscle weakness: Since our nerves are responsible for stimulating our muscles, you may experience reduced strength and control in the muscles connected to the affected nerve.
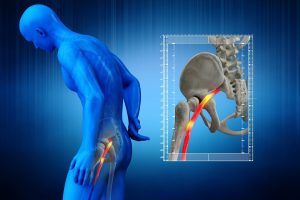
- Radiating pain: Discomfort that extends beyond the initial site of compression. In the neck, it may go down into the shoulder blade or down the arms into the fingertips. In the lower back, it may radiate down into the glutes or further down to the legs or feet.
Why does physiotherapy help?

Manual therapy is one of the treatment techniques used by physiotherapists to relieve pain and increase mobility
Physiotherapy is the first line of treatment for a pinched nerve. It is non-invasive and has shown to be an effective approach for managing pain and dysfunction from a pinched nerve. A skilled physiotherapist can create a tailored treatment plan to address the specific needs of each individual. A treatment plan may include some or all of the following:
- Manual Therapy: Hands-on techniques such as joint mobilization and soft tissue manipulation can help alleviate pressure on affected nerve. These techniques can help stiff areas, subsequently improving mobility and reducing pain.
- Exercise Prescription: Targeted exercises may include stretches or postures to help relieve pain and other symptoms. Once the pain has been controlled, strengthening the muscles near the area of the affected nerve will help minimize the risk of future reoccurrences.
- Posture Correction: Addressing poor posture is crucial in preventing and managing pinched nerves. Oftentimes, a certain position can be aggravating for the neck or back. A physiotherapist can assess which positions are helpful or harmful to you, and provide guidance on how to incorporate these changes into your daily life.
- Education: Understanding the factors contributing to pinched nerves is essential for long-term management. Your physiotherapists will help you understand the do’s and dont’s during your treatment, and the predicted timeline of your recovery.
- Modalities: Therapeutic modalities such as ultrasound, electrical stimulation, or heat and cold therapy may be helpful in reduce inflammation and reducing pain.
Need help? Look for PhysioNow!
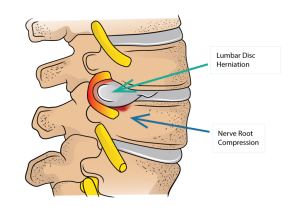
Lumbar disc herniation resulting in a pinched nerve can be quite common, but may be treated with physiotherapy.
Pinched nerves may sound intimidating but with the right approach, they can be effectively managed. Physiotherapy offers personalized care to enhance mobility, alleviate pain, and improve overall quality of life. If you suspect a pinched nerve or have low back pain, PhysioNow is here to help! Consult with our expert team of physiotherapists with locations across the GTA. Book with PhysioNow today for your first assessment and treatment.