Why is your ankle sprain not healing?
 An ankle sprain is one of the most common injuries. Rest, ice, compression, and elevation, or the RICE rule, will be the go-to’s for ankle sprains. In most cases, ankle sprains heal between 4-12 weeks depending on the severity of the injury. Though many people will have them to heal with time. However, a failure to seek treatment and physical rehabilitation for your ankle after just one injury is enough to leave it weak. This makes your ankle more vulnerable to future sprains or chronic instability.
An ankle sprain is one of the most common injuries. Rest, ice, compression, and elevation, or the RICE rule, will be the go-to’s for ankle sprains. In most cases, ankle sprains heal between 4-12 weeks depending on the severity of the injury. Though many people will have them to heal with time. However, a failure to seek treatment and physical rehabilitation for your ankle after just one injury is enough to leave it weak. This makes your ankle more vulnerable to future sprains or chronic instability.
What causes you chronic instability after an ankle sprain?
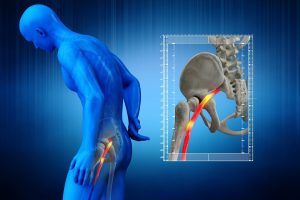
After an ankle injury, there is damage to the ligaments, tendons, and potentially even the ankle joint itself. Here, the function of the ligament is to limit abnormal movement in the joint. Because of the injury, they will get lax (stretched out), making the ankle more unstable. Additionally, this will also result in a loss of strength in the muscles, further increasing the instability of the ankle. Also, sensory receptors are impaired which communicate to our brain where your ankle is or where it is relative to the rest of our body. At last, this decreasing sensation makes it hard to balance and control the ankle which will have contributes to ankle instability.
How do you know if you have instability post ankle sprain?
Consider the questions below if you ever sprained your ankle and feel weak.
• Does your ankle ever give out?
• Avoid walking on uneven surfaces out of fear of falling?
• Feel like you can’t “trust” the ankle?
• Try to avoid putting all your weight onto one ankle?
If you said yes, to these questions and you may have chronic ankle instability.
Is it permanent?
Chronic ankle instability is not permanent. You can improve your ankle stability with the help of a physical therapist and an individualized exercise plan. But, If the injury is left treated it results in chronic instability and vulnerability to injuries. In this case, the first step to treatment will be a proper rehabilitation program with a health professional.
How to treat your unstable and weak ankles?
Physical therapists are the first step in the conservative management of chronic ankle instability. Due to loss of strength and proprioception, rehabilitation is very important. They perform a complete assessment of your ankle range of motion, strength, and balance assessing for any laxity, or any abnormalities, and guide you through the management.
 Exercises re-strengthen the muscles, increase ankle stability, and balance, and retrain the body awareness of the ankle. Moreover, Brace and/or taping may be recommended to support the stabilization of the ankle, especially for individuals who are engaged in high-risk activities like sports.
Exercises re-strengthen the muscles, increase ankle stability, and balance, and retrain the body awareness of the ankle. Moreover, Brace and/or taping may be recommended to support the stabilization of the ankle, especially for individuals who are engaged in high-risk activities like sports.
Next, surgery may be an option to repair the injured ligaments if there is any tear or fracture is sustained.
What happens if your ankle sprain and injury are left untreated?
The instability may worsen over time and you will have a much greater risk of reoccurring injuries. In addition, it results in damage to the bones and cartilage within your ankle joint as the muscles weaken and fail to sufficiently support the joint. Therefore, it is highly recommended that you seek treatment from an expert to treat the issue before it results in a severe injury.
If you are having any instability or weakness with your ankle, which is stopping you from pursuing any hobbies book with PhysioNow today for an initial assessment and treatment. We have a team of highly qualified physical therapists that will be able to help your ankle recover!