Pickleball has exploded in popularity in the last couple of years across North America, with outdoor courts and racquet clubs popping up everywhere. The appeal is obvious as a fun, competitive or casual, social sport that can accommodate all ages and fitness levels. Whether you’re previous athlete or just trying for the first time, the greatest draw of pickleball is it’s accessibility. As Physiotherapists, we have also encountered a lot more pickleball-induced injuries recently. In this blog we’ll discuss the most common ones we see and a couple of tips to help you stay injury free this summer!
What are common pickleball injuries?

Pickleball is a sport with fast movements, quick changes in direction or starting and stopping, and repetitive plus powerful arm motions. As a result, the most common injuries tend to be:
- Rotator cuff strains/sprains: Either an overuse or acute injury, overhead shots and smashes put a lot of strain through the shoulder joint and muscle
- Knee strains/sprains: Overuse injuries can be like ITB syndrome, PFPS from muscular imbalances, or more acute injuries from sudden movements like a ligament or meniscal injury
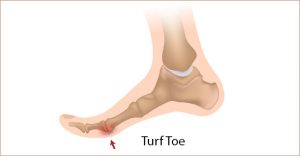
- Ankle ligament sprains: Common methods of injury include rolling/twisting your ankle, landing from a jump, or starting/stopping movement too quickly
- Tennis/golfer’s elbow: This is an overuse injury of the muscles of the forearm, where a lot of the strain from holding and swinging the racket is directed
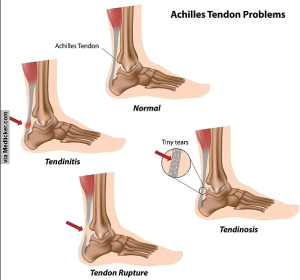
- Achilles tendon problems: The strongest tendon in our body at the back of our heels, it is responsible for absorbing the stress of jumping, landing, changes in direction, running and more. Issues can be acute or from overloading the tendon
Staying injury-free with Physiotherapy
Physiotherapists are movement experts, and whether it is rehabilitation, injury prevention, or optimizing performance, we can help you with your game! Our recommendations for our pickleball athletes are as follows:
1. Ensure that your equipment and footwear is in good shape
Poorly maintained or fitting equipment can greatly increase your risk of injury. Ensure that your shoes fit well and provide enough grip to prevent slipping on the court.
2. Have a movement analysis done
Whether by a Physiotherapist or a coach, they can evaluate your technique and help you identify any issues. They can assess your movement patterns, running, jumping, swing, and how you hold your paddle For example, improper or over gripping can change the amount of stress on the forearm muscles and predispose them to injury.
3. Engage in a cross training routine
We highly recommend engaging in cross training, especially the more frequently you begin to play pickleball. Cross training helps to give the muscles primarily stressed by pickleball some rest, while still allowing you to work towards getting stronger, faster, and more cardiovascular fitness. While it may be tempting to play pickleball everyday, remember that your body needs a rest as well to repair itself. Cross training activities we recommend include resistance/weight training and another form of lower impact cardio like the elliptical, rowing, or swimming.
4. Regular body maintenance
If you’re playing often, we recommend some focus on recovery whether its through Massage Therapy, Physiotherapy, or Manual Osteopathy. Not only does this help with injury prevention, but it can help you understand and engage in techniques like active recovery, soft tissue work or stretching and mobility work to reduce muscle inflammation and soreness.
5. Treating old injuries and impairments
It is important to address any pre-existing issues or injuries to ensure you’re in the best shape to play. For example, individuals who have had previous shoulder problems or lack mobility/strength in their shoulders are more likely to develop pain due to overuse in their forearm. As can be seen, a weakness in one area requires compensation with a different area of the body. Alternatively, If you are someone who struggles with mobility and has a hard time getting their arms overhead and behind your ears, you’re going to have a hard time hitting those overhead shots. Physiotherapy can help you work on these problems with a personalized treatment and training protocol.
Ready to level up your pickleball game?
Look for PhysioNow! We have many expert professionals (many of which love pickleball themselves!) that are ready to help you on your journey. Whether you’re looking for help with an injury, prevention, or looking for performance tips, we can help. Book with PhysioNow today for your first assessment and treatment. We have 10 locations across the GTA from Burlington, Oakville, Mississauga, to Etobicoke ready to serve your needs!
Images by FreePik