In the athletic world, sports injuries are a common occurrence while participating in competitions, organized sports, fitness activities, or training exercises. For starters, poor training methods, a lack of conditioning, and/or inadequate warm-ups are a few of the causes of sports-related injuries. At certain times, coping with these kinds of injuries often calls for physical rehabilitation.
Physical therapy helps people regain strength and movement in parts of their body after an injury. Additionally, it can help someone manage their pain and prevent permanent damage and recurring problems.
What are some examples of sports injuries?
Firstly, common ways that athletes get hurt depend on the kind of sports they participate in. They may be at risk for one or more of these kinds of injuries:
-
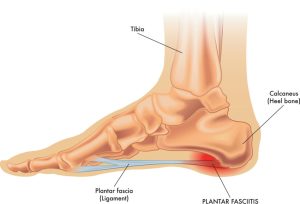
Ankle injuries
— Just about any athlete who is on their feet a lot is at risk for an ankle injury. If the athlete rolls their ankle or if they twist it, it can strain or tear the tissue.
-
Pulled muscles
— Overusing the muscles, especially muscles that are tired after a long period of use and performance can cause them to over stretch or tear.
-
Shin splints
— Running for long hours can cause the muscles and connective tissue around your shin to get inflamed.
-
Knee injuries
— A sharp twisting of the knee or bending it in the wrong way can cause a sprain to the ligaments in your knee.
-
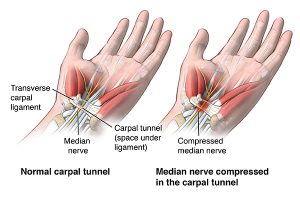
Tennis elbow
— Known officially as lateral epicondylitis/epicondylalgia, tennis elbow happens when the muscles and connective tissues around your elbow become inflamed from overuse.
-
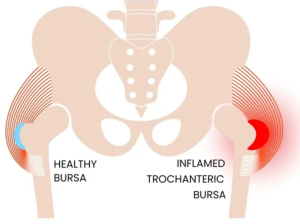
Hip Flexor Strain
— The hip flexors are muscles located on the upper-front side of your thigh. Typically, injuries to these muscles are caused by sprinting, running inclines and activities with sharp turns and/or sudden starts.
-
Concussion
– These are traumatic head injuries that may result in severe headaches and altered levels of alertness and consciousness. Usually, they occur when a moving object hits the head or the head hits an object. Unfortunately, concussions are one of the most difficult-to-manage injuries in sports today. Ultimately, physical therapy is an integral part of the multidisciplinary approach to the diagnosis and treatment of concussions.
Preventing Sports Injuries:
Physical therapy is not just about treating injuries—it’s also a powerful tool for injury prevention. By improving athletes’ strength, flexibility, and coordination, physical therapy can help to make
athletes more resilient and less prone to injury.
Prevention strategies include targeted strength and conditioning programs to bolster weak areas and improve overall physical performance. Furthermore, physiotherapists provide valuable education on proper technique and body mechanics, both in general movement and sport-specific skills. Corrective exercises can be used to address any biomechanical abnormalities that may increase the risk of injury. Overall, this training helps athletes to move in safer, more efficient ways, significantly reducing the risk of injury.
Treating Sports Injuries:
Physical therapy plays a multifaceted role in treating sports injuries. At the core, physical therapy helps in the restoration of function, improving mobility, and relieving pain. Physiotherapists employ
a variety of techniques to achieve these goals. Importantly, these are customized based on the nature and extent of the injury and the specific needs of the athlete. Therapeutic exercises are used to strengthen weakened muscles, improve flexibility, and restore
range of motion.
Furthermore, modalities such as heat and cold therapy, electrotherapy, and ultrasound may also be
used to stimulate tissue healing, reduce pain, and decrease swelling.
Where can I get help with sports injuries?
At Physionow, we adopt a personalized approach to sports injury rehabilitation. The process begins with a comprehensive assessment, which helps us to develop a tailored rehabilitation plan that includes a combination of therapeutic exercises, and other physiotherapy techniques as needed. Overall, the goal is to facilitate healing, restore function, and improve performance.
However, rehabilitation doesn’t just stop at injury recovery. We also strive to prevent future injuries. This involves providing education on injury prevention, recommending sport-specific conditioning programs, and teaching proper body mechanics. Our treatment is comprehensive, personalized, and focused on helping athletes return to their sport safely and confidently.
Book with PhysioNow for your first treatment and assessment today! We have 9 locations across the GTA including Burlington, Oakville, Mississauga and Etobicoke.