What is the Achilles tendon?
The Achilles tendon is one of the strongest tendons in the human body. Anatomically, it connects our calf muscles to the back of the heel bone. Its main action is to point the toes and ankle downwards when our foot is off the ground or raise the heel off the ground when our foot is on the ground.
Functionally, it is used whenever we are engaged in walking, running, or hopping-like activities and helps us with force production and shock absorption. The tendon is extremely strong and can withstand high amounts of stress Unfortunately, this can also predispose it to injury and cause ankle pain.
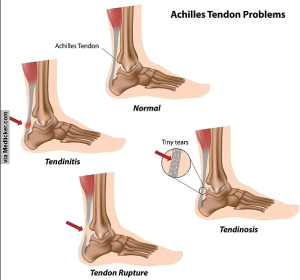
Stages of Achilles tendon injuries
1) Achilles tendinitis: Inflammation has developed or is developing in the tendon.
2) Achilles tendinosis: There is now degeneration along with or as a byproduct of the inflammation. This is usually an issue that takes a long time to occur. For example, if an Achilles tendinitis is left untreated for months, it can eventually transition into the tendinosis.
3) Achilles tendon tear or rupture: As the tendon fibers are weakened from the tendinosis, it increases the chance that they can tear entirely.
What is Achilles tendinitis?
Achilles tendinitis means inflammation has developed in the tendon. Potentially, due to overuse of the tendon or a trauma like a fall or sport injury. Inflammation is the human body’s natural and healthy reaction to any kind of injury or disease. However, when it lasts for too long it can start to have negative effects. The inflammation can be rated as minimally painful to severely painful. At this last stage is where a patient’s walking ability can be compromised.
Causes of Achilles tendinitis:
1) Trauma: Direct trauma on ankle during car accident, fall etc
2) Running, dancing, jumping: Constant high impact movements increase the risk of injuring the Achilles tendon
3) Flat feet: Having flat feet may change the weight distribution in the foot and put extra pressure on the tendon
4) Playing Sports: Playing less frequent sports does not allow their body to take pressure regularly and increases the chances of injury
5) Heavy standing job: Constant being on feet increase the chances of injury
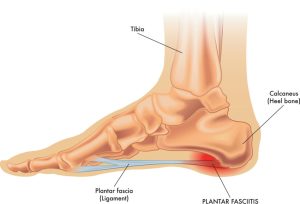
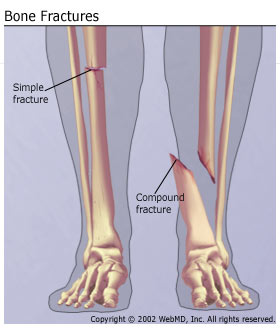
6) Bony spur in heel / Plantar Fasciitis/ Ankle fracture:
Extra fluid from swelling or bony protrusions in the ankle can rub against the tendon causing an injury.
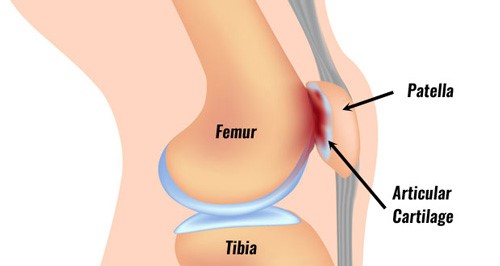
7) Calf, knee, or hip muscles weakness:
Muscle strength imbalances can cause compensations in the tendon and increase the stress it is exposed to.
Sign and symptoms of Achilles tendinitis:
1) Pain and inflammation in back of heel bone
2) Stiffness and tenderness in ankle
3) More pain after any strenuous activity
4) Leg weakness
5) Worse in the morning, might improve as day goes by
Diagnosis
Book your assessment with a registered physiotherapist. They will assess your posture, leg alignment, range of motion of joints, muscular strength and determine the source of your pain.
Additionally, diagnosis may be achieved through imaging like Diagnostic Ultrasounds and MRIs.
How do I treat it?
In the beginning, non-invasive therapy will help to treat the condition.
1) RICE protocol
Rest: Stop doing activities that stress your tendon. Switch to low-impact activities, such as swimming, that put less stress on the Achilles tendon.
Icing: Put ice on your tendon for up to 20 minutes, as needed throughout the day.
Compression: Compress, or put pressure on, the tendon using an athletic wrap or medical tape.
Elevation: To reduce swelling, lie down and raise your foot on pillows so it’s above the level of your heart.
2) Shockwave therapy:
Shockwave therapy may help improve the condition, especially for stubborn conditions that have lasted over 6 weeks.
3) Physiotherapy:
Muscle release, stretching and strengthening exercises will help improve the tendinitis.
4) Orthotics:
Proper footwear and the use of custom orthotics will help support the foot and ankle, putting less stress on the tendon.
Achilles pain? Look for PhysioNow!
If you are looking for treatment for your Achilles pain, or any other type of foot, ankle, or sport injury, look no further. PhysioNow has many expert Registered Physiotherapists prepared to help you with diagnosis, treatment, orthotics, bracing, shockwave therapy and more. With locations across Burlington, Oakville, Mississauga , and Etobicoke we have you covered. Book PhysioNow today for your first assessment and treatment.