What is a total hip arthroplasty?
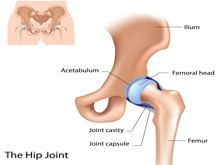
Total Hip Arthroplasty (THA), or a hip replacement surgery is a procedure that replaces damaged bone and cartilage in the hip joint. Instead, it replaces it with prosthetic components mainly using two techniques. The type of technique used will be discussed between you and your surgeon and is influenced by demographic and lifestyle factors.
1: Cemented: Used more in geriatric (older) populations or patients who have a more sedentary lifestyle
2: Non-cemented: Indicated for younger populations, or patients having active lifestyles
Why do people get hip replacements?
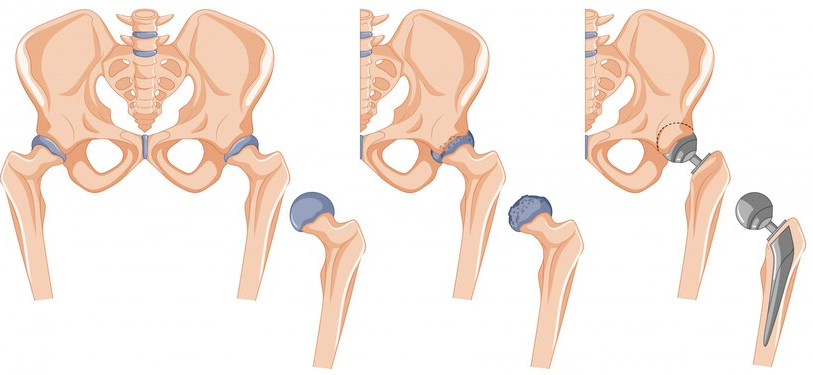
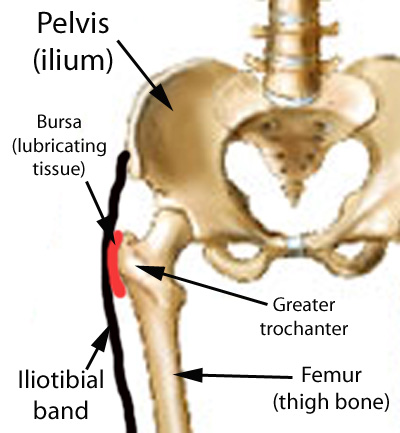
Usually, the reason people get hip replacement is due to severe osteoarthritis (OA) that is causing high pain, loss of function, and disability. For example, when someone is having trouble walking and being independent with their daily activities due to issues with hip OA. Other reasons may include rheumatoid arthritis induced cartilage or bone damage, after a slip and fall on the hip (especially in older populations), and femoral neck fractures. However, some people may be ineligible for this surgery if they have peripheral vascular disease, history of blood clots, an ongoing infection, or septic arthritis.
Generally, hip replacements/THAs are safe procedures with great outcomes. Post-surgery, the most common complications to watch for include deep vein thrombosis which is a blood clot in the leg, or a post-surgical infection in the joint.
Physiotherapy Rehabilitation After Total Hip Arthroplasty
Total hip arthroplasties are highly effective surgical procedures designed to alleviate pain and restore function in patients with severe hip arthritis or hip joint damage. Initially, post-operative rehabilitation is crucial to ensure the continued success of the surgery and to optimize the patient’s recovery. Physiotherapy plays a vital role in this rehabilitation process, helping patients regain strength, mobility, and overall function. Read on to learn more about the phases of rehabilitation with Physiotherapy!
1. Immediate Post-Operative Phase
First, the immediate post-operative phase begins as soon as the patient wakes up from anesthesia. Then, physiotherapists start with gentle exercises to promote blood circulation and prevent complications such as deep vein thrombosis (DVT). Simple movements like ankle pumps, quadriceps sets (squeezing the big thigh muscle), and gluteal sets (squeezing the buttocks muscles) are encouraged. These exercises are designed to improve blood flow, reduce swelling, and initiate muscle activation without putting undue stress on the new hip joint.
Early mobilization is a critical component during this phase. Within 24 to 48 hours after surgery, patients are usually assisted to sit up and begin walking with the help of a walker or crutches. The goal is to start weight-bearing activities as tolerated, promoting healing and preventing stiffness.
2. Early Rehabilitation Phase
The early rehabilitation phase spans the first few weeks after surgery. During this period, physiotherapists focus on gradually increasing the intensity and range of exercises. Patients are taught specific hip-strengthening exercises such as leg raises, hip abductions, and gentle stretching. Additionally, simple balance and coordination exercises are also introduced to enhance stability and prevent falls.
Not only this, but pain management is a significant focus during this phase. Physiotherapists work closely with the medical team to ensure that pain is adequately controlled, allowing patients to participate actively in their rehabilitation. For example, ice therapy, electrical stimulation, and manual techniques may be used to manage pain and reduce inflammation.
3. Intermediate Rehabilitation Phase
The intermediate phase, typically from 4 to 12 weeks post-surgery, aims to build on the progress made in the early phase. Now, physiotherapy sessions become more intensive, incorporating resistance training and functional exercises. Furthermore, activities such as stationary biking, swimming, and gentle aerobics are introduced to improve cardiovascular fitness and endurance.
During this phase, the focus shifts towards improving gait and mobility. For example, patients practice walking without assistive devices, concentrating on proper walking mechanics and posture. Also, stair climbing and descending exercises are introduced to further enhance functional independence.
Strengthening exercises for the hip and surrounding muscles are progressively intensified. At the same time, core strengthening exercises are also incorporated to improve overall stability and support the hip joint.
4. Late Rehabilitation Phase
The late rehabilitation phase, typically beyond 12 weeks post-surgery, focuses on preparing the patient for a return to normal activities and, if possible, sports. Now, physiotherapy sessions aim to restore full strength, flexibility, and function. Advanced balance and proprioception exercises are introduced to ensure the patient can handle more complex movements and environments.
At this stage, patients may engage in low-impact sports such as golfing, cycling, and swimming. High-impact activities, such as running or jumping, are generally discouraged to protect the new hip joint from excessive wear and tear. However, each hip rehabilitation is different and should be discussed with your surgeon to understand your specific limitations.
Education on lifelong joint protection and healthy lifestyle choices is an essential part of this phase. Patients are taught strategies to prevent injury and maintain joint health, such as maintaining a healthy weight, avoiding high-impact activities, and incorporating regular exercise into their daily routine.
Getting a hip replacement soon?
If you are getting a total hip replacement soon and are looking for some advice and help, look for PhysioNow! Physiotherapy can help you maximize your strength and function prior to surgery to ensure that recovery is as smooth as possible. Then, after the surgery, we will work with you to return your hip back to its normal function with an individualized care plan. Our Physiotherapists are ready to get you started. Book with PhysioNow for your first assessment and treatment today!