Vaginismus and Physiotherapy
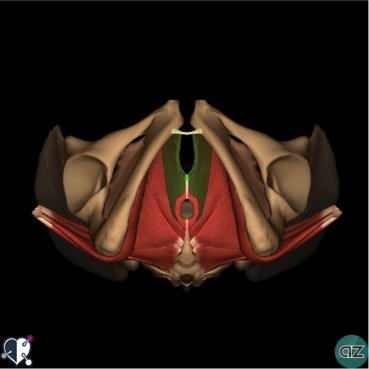
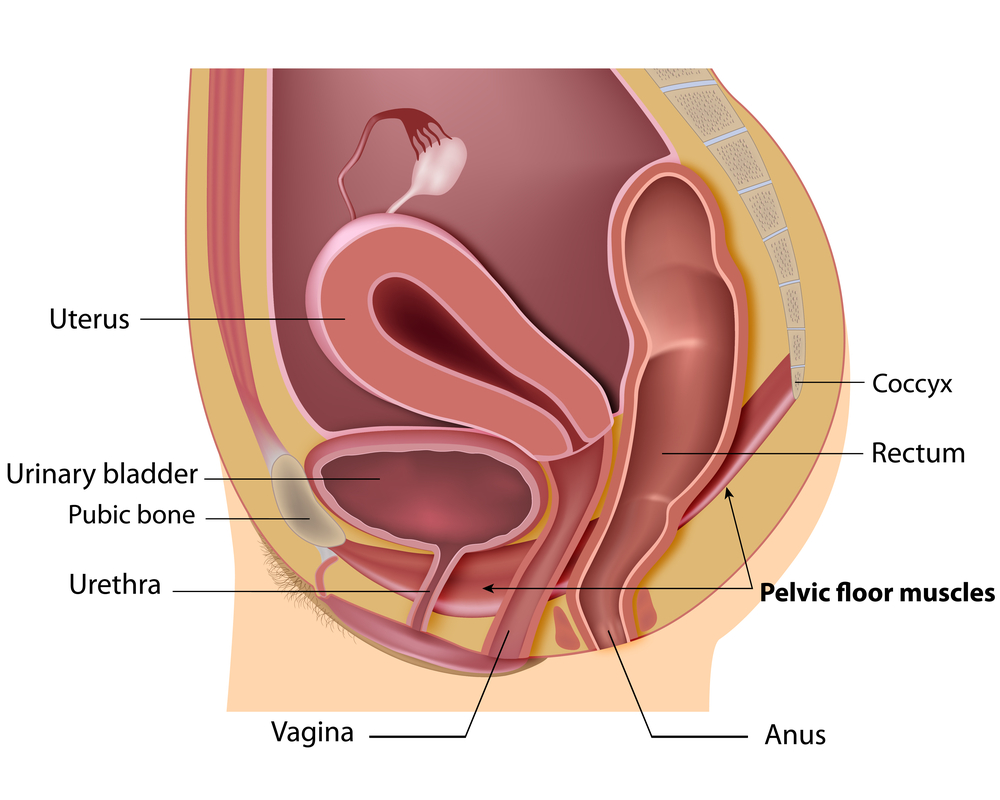
Vaginismus is a painful feeling of discomfort or inability when inserting a tampon, finger, penis or during a doctor’s internal pelvic exam. It occurs when there are involuntary contractions of the muscles in the outer third of the vagina.
Primary Vaginismus: when a woman has never been able to have pain free intercourse due to pelvic floor muscle spasm.
Secondary Vaginismus: pain that develops sometimes later in life after a traumatic event such as childbirth, surgery, or a medical condition.
With Vaginismus, there is usually significant Connective Tissue Dysfunction that needs to be addressed first before any internal work. It is suggested that you follow up the self-help treatment for connective tissue dysfunction before embarking on the stretching exercises with the dilators.
Pelvic floor exercises and Desensitisation techniques
A physiotherapist may be able to teach you pelvic floor exercises, such as squeezing and releasing your pelvic floor muscles, that can help you gain control over the muscles causing the vagina to close involuntarily. Occasionally, a technique called biofeedback may be useful. A small probe is inserted into your vagina. This monitors how well you are doing the exercises by giving you feedback as you do them.
Biofeedback can help with the following:
• Teach you strategies that may help to relax the muscles that are contracting involuntarily
• Teach you appropriate timing of the contraction and relaxation of the pelvic floor muscles.
• Educate you about your condition and why it might be occurring.
• Teach you various strategies for getting the muscles to relax
• help you to Use manual therapy to release the muscles either externally and/or internally that are causing the contractions.
More information about Vaginismus can be found here.
Some general tips about pelvic floor muscle exercises:
• Choose a convenient time and place where you can exercise regularly.
• Put a reminder about pelvic muscle exercises somewhere obvious to you (or set an alarm on your watch or mobile phone).
• Avoid quick pelvic floor muscle exercises where you don’t hold the contraction. This tends to cause an increase in pelvic floor muscle resting tone.
• Be aware that it will take 6 to 8 weeks of regular exercise before you can expect to see improvement. It will take approximately 3 months for the pelvic muscles to strengthen.
• You could try inserting one finger into the vagina to check the strength of your squeeze as you pull in the pelvic muscles. Alternatively, you may be able to feel a pelvic floor contraction if you place the tip of your index finger on the perineal body (on the outside, between the vagina and back passage).
Other tips to reduce Vaginismus:
• If you are overweight, try reducing your weight.
• Try not to become constipated, as a full bowel will put pressure on the bladder. Straining to empty your bowel will weaken the pelvic muscles.
• If your job involves lifting, think of your pelvic muscles as well as your back. Pull up your pelvic muscles when lifting a heavy weight.
• If you smoke, consider quitting. Frequent coughing puts a strain on the pelvic muscles.
If you or someone you know suffers from Vaginismus, please call PhysioNow today! Our specially trained Physiotherapist can start your treatment Now!
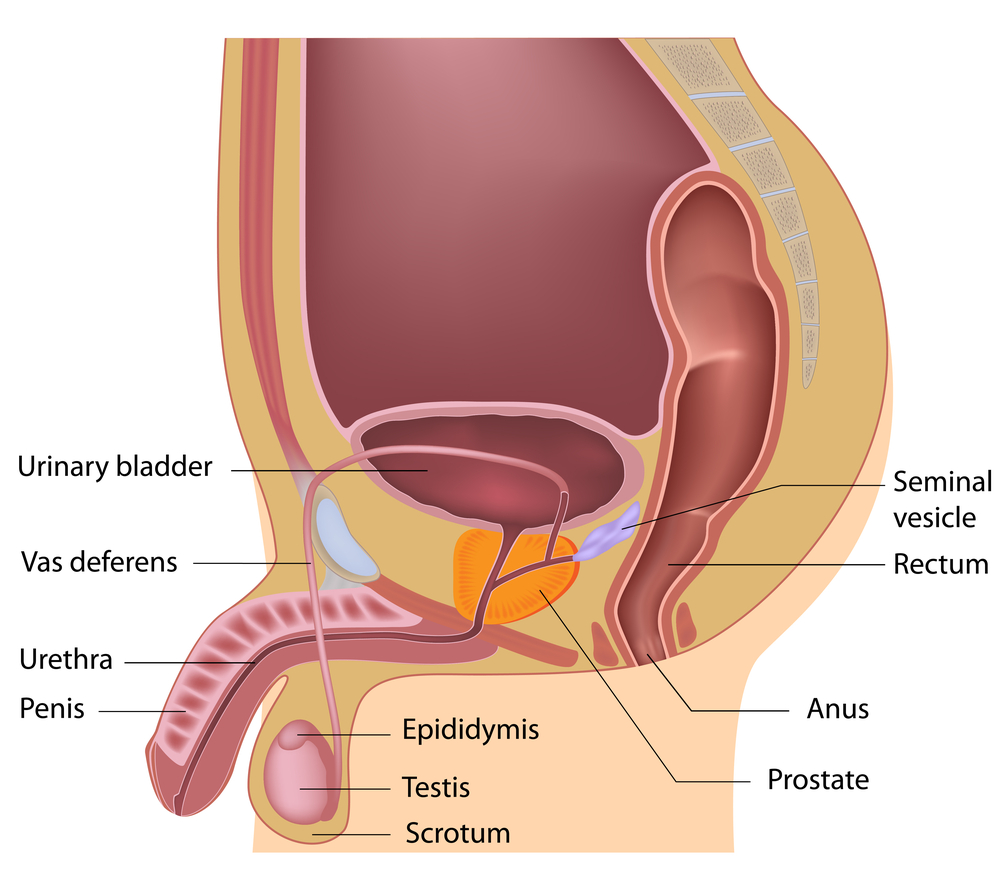
 Female & Male pelvic pain
Female & Male pelvic pain