What happened to Kevin Durant?
Kevin Durant originally injured his calf in early May during the second round of playoff games. The injury had been labeled a ‘calf injury’ and Durant has not been able to play for over 30 days. After doing a shoot around with the team, the Warriors made the decision to allow Durant to play for Game 5. Durant came out strong, scoring 11 points in 12 minutes of play. But things changed as he tried to do a crossover move and had to fall to the floor on the sidelines. He was grabbing onto his lower right calf, more towards his Achilles tendon. In conclusion, from the replays, it looked like he may have torn his Achilles tendon.
What is the difference between a calf strain and an Achilles tendon tear?

Kevin Durant’s injury
Calf Strain : Did Kevin Durant have this injury?
It is possible that Kevin Durant had a calf strain to start.
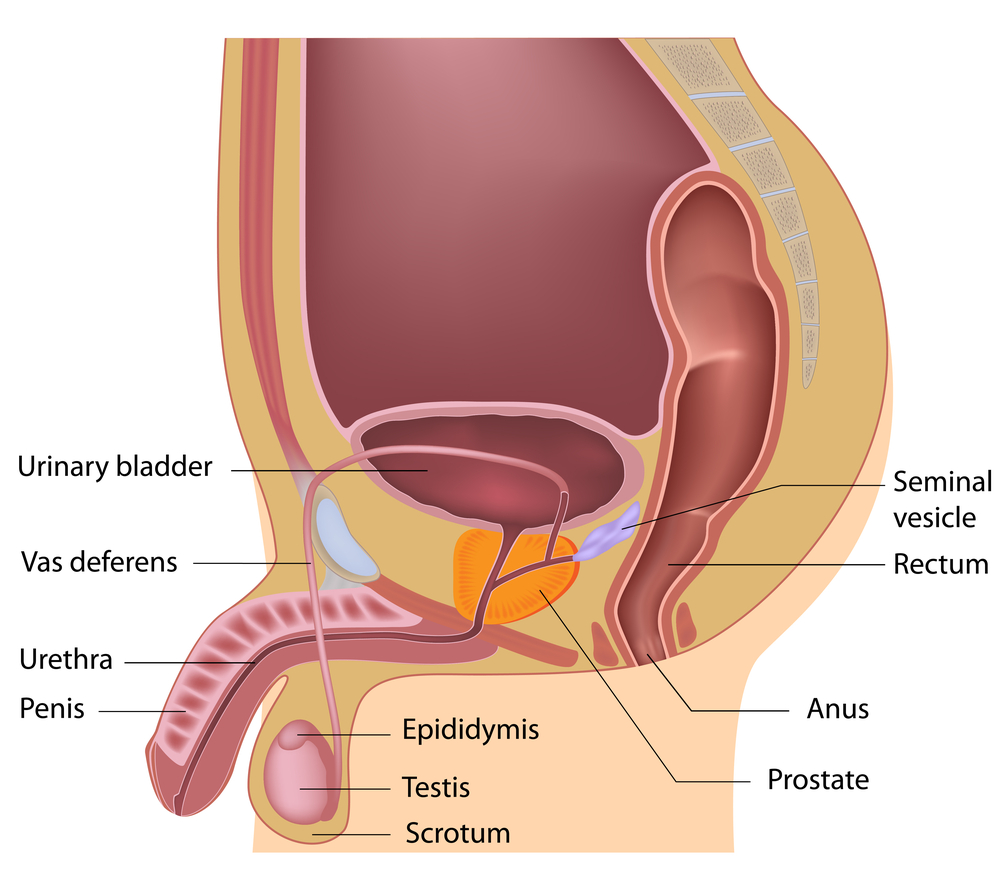
The bulk of the calf is made up of 9 different muscles. Three muscles work together to produce a downward movement of the foot. These 3 muscles attach themselves into the heel bone:
- Gastrocnemius
- Soleus
- Plantaris
Other Muscles of the calf/ foot
The other 6 muscles cause knee, toe and foot movements in different directions. These muscles are located deeper in the calf area. However, these muscles travel around the sides of the ankle and attach to different parts of the foot and toes. These muscles are:
- Popliteus
- Flexor digitorum longus
- Flexor hallucis longus
- Tibialis posterior
- Peroneal longus
- Peroneal brevis
Sometimes injuries are labelled incorrectly. Pain in the calf region is attributed to the first three muscles. However, a calf strain could involve any one of the 9 muscles mentioned above. As a result, it is up to the health professional to correctly identify which of the muscles are involved in the strain.
Severity of Calf Strain: What Grade did Kevin Durant have?
In general, a calf strain is caused by overstretching or tearing of the calf muscles. This type of injury can occur suddenly or over time. The severity of the strain is graded by the amount of muscle damage that has occurred:
- Grade 1
- Mild or partial stretch or tearing of a few muscle fibres
- The muscle may be tender and painful
- Strength and function are maintained
- Grade 2
- Moderate stretching or tearing of a greater percentage of muscle fibres
- A snapping or pulling sensation may be felt at the time of the injury
- More tenderness and pain
- There may be some visible bruising
- Loss of strength and function
- Lastly, Grade 3
- Severe tear of the muscle fibres, commonly a complete rupture
- A ‘popping’ sound may be heard of felt at the time of the injury
- There is definite bruising and sometimes there is a visible ‘dent’ in the muscle
- Severe loss of strength and function
Signs and Symptoms of a Calf Strain
- A snap, pull or “pop” felt or heard at the time of injury
- Pain and weakness in the calf area
- Swelling in the calf area
- Tightness
- Bruising
- Weakness in the calf when doing any weight bearing activities
- Limping when walking
What is the usual Physiotherapy treatment for a calf strain?
Treatment for a calf strain is like that of any other muscle in the body. The goals of the treatment include:
- Reducing pain
- Improving range of motion of the knee and ankle
- Improving the strength
- Speeding up recovery time
- Returning to activities
- Preventing re-injury
How long does it take to recover from a calf strain?
The length of time for recovery from a calf strain injury depends on the severity of the injury. On average:
- Grade 1: 10-12 days
- Grade 2: 4-6 weeks
- Lastly, Grade 3: 6 months after surgery
Achilles Tendon Rupture : Kevin Durant’s final injury
The gastrocnemius, soleus and plantaris muscles unite to form the Achilles tendon. The tendon is a tough band of tissue that connects these three calf muscles to the heel bone. When the calf muscles contract, the Achilles tendon is tightened and pulls the heel. As a result, the action allows the foot to be pointed down. A complete tear of this tendon is called an Achilles tendon rupture.
Signs and symptoms of Achilles Tendon Rupture
- Sudden and severe pain at the back of the ankle or calf
- Sound of a loud pop or snap
- Immediate swelling and weakness
- Visible bruising and possible denting in the tendon
Treatment options for Kevin Durant’s Achilles Tendon Rupture
- Non-surgical treatment
- Rest
- Crutches
- Ice
- Pain medication
- Immobilisation for the first few weeks with a walking boot and heel wedges
- Recovery may take longer but risks of surgery are avoided
- Surgical Treatment
- Involves making an incision in the calf and stitching together the torn tendon
- Minimally invasive surgical techniques are available
- Risks of surgery include possible infection and nerve damage
- check out this link that further discusses the surgical option https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/achilles-tendon-repair-surgery
The choice between surgical or non-surgical treatment depends on different factors. A patient’s age, activity level and severity of the injury all play a factor. In general, younger and more active people, especially athletes, choose surgical repair. In contrast, older and more sedentary individuals usually choose the non-surgical pathway. In either option, rehabilitation is a lengthy and difficult process to make sure full function is returned.
So, what happened to Kevin Durant?
The Kevin Durant was out for over a month with an initial calf strain. Due to the amount of time that he was out of the game, it’s likely that he had a grade II strain of his calf. As a result, his return to the game resulted in a complete Achilles tendon rupture. In review, it makes you wonder whether he was physically able to return to play. Did he have enough time for recovery from his initial injury to withstand the demands of the game?
Basketball is a sport that has a lot of pivoting, stop and go movements and bursts of high intensity activity. In conclusion, it is possible to say that judging from how soon into the game the injury happened, that Kevin Durant was likely not fully recovered.
Professional Sports: Decisions for return to play. Should Kevin Durant have returned to play in Game 5?
However, in professional sports, there is a lot of pressure from all fronts to get a star player back in the game. The team was down 3-1 and having Durant back in the game boosted their confidence and morale. As a result, the fans wanted the Warriors to win. The organization wanted the team to hold on to their title again. In addition, Kevin Durant himself probably felt terrible that he wasn’t able to play and support his team. As a result, all of these pressures likely led to the decision for him to play.
Unfortunately, our bodies are not always able to function like we want them to. In Durant’s case, his return to the game led to an even more serious injury, which required surgery. In conclusion, after surgery he will have to endure a lengthy process of physical therapy and will likely be out for the entire next season.
Return to Play Decisions
This is an excellent example of the importance of return to play decisions. Regardless of the sport and regardless of the injury, it is vital that the health and well being of the athlete is the top priority. In conclusion, returning to play too soon isn’t worth risking a more serious injury. Lastly, a more serious injury can affect the athlete’s future participation in the sport.
Physiotherapy Treatment options for Achilles Rupture
If you or someone you know has experienced calf pain or an achilles rupture, our Physiotherapists at PhysioNow are here to help! We have treated many patients with exactly these injuries. Call today to get started on your treatment and get back in the game!