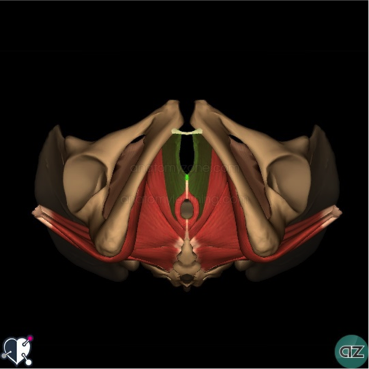
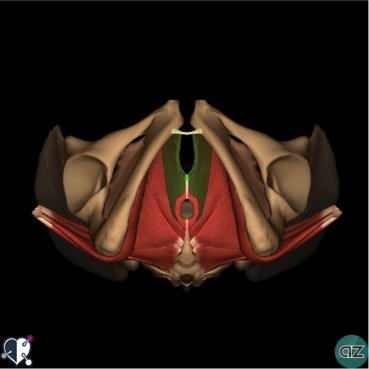
PELVIC PAIN AND PELVIC FLOOR DYSFUNCTION
What is pelvic pain and pelvic floor dysfunction?
There are a number of conditions which cause pain and pelvic floor dysfunction. We have discussed a few of those conditions here today. Fortunately most of the conditions are treated with physiotherapy interventions.
Common conditions related with internal pelvic structures:
Provoked vestibulodynia: In this your pelvic area is very sensitive to touch or pressure. You will feel pain with
- light touch,
- pressure,
- inserting tampons,
- wearing tight pants or
- intercourse.
- urinary urgency
Vaginismus: You feel difficulty and/or pain with vaginal penetration. This will lead to avoidance of sexual activity or internal pelvic examination.
Bladder pain syndrome: You feel pain and pressure with urge to urinate at any time. You will get an increased urge to urinate. Symptoms usually starts with bladder infection.
Dysmenorrhea: You will feel painful cramps with mensuration. It affects about 90% of the women. This could include pelvic adhesions, pelvic inflammatory disease and cervical stenosis.
Conditions related to activities and damage to structures:
Dyspareunia: It is pain with sexual intercourse. Damage to the structures like:
- episiotomy,
- tears,
- reduced mobility of cervix or soft tissues,
- bladder pain,
- overactive muscles and
- inflammation
Coccyx pain: It is the pain in tail bone are with sitting, sit to stand, sexual activity, or with bowel movements. Usually caused by any trauma, inflammation or muscle imbalance.
Conditions involving neurological structures:
Pudendal Neuralgia: There is pain and numbness in the area supplied by nerve from anus to penis or clitoris. You will feel pain with sitting, fecal and urinary incontinence. There are other underlying conditions that can restrict your pelvic mobility. This leads to compression of your pudendal nerve.
Male pelvic pain issues:
Certain conditions such as dysfunction of pelvic muscles, non-bacterial inflammation of prostate, Pudendal neuralgia, anal fissures, Coccydynia, bladder pain causes pelvic pain in male patients.
If you want more information about the conditions which cause pelvic pain visit this link https://www.onhealth.com/content/1/pelvic_pain_causes
Experiencing any of the above symptoms?
Pelvic floor therapist helps you with thorough assessment and treatment based on the diagnosis. Educating you about the cause of the pain. Managing with home exercise program.
Treatment techniques done by pelvic floor physiotherapists:
For vestibulodynia:
Physiotherapy is considered as the first line of treatment for you. Your physio will treat with tissue care, manual techniques for painful points, muscle imbalance, relaxation techniques. You will learn to avoid wearing tight clothes and diet modification.
For Dyspareunia:
Relaxation techniques along with dilator insertion helps to relieve tension in the vaginal area. Pelvic therapist will releases scar tissue in the vaginal area which reduces pain. Soft tissue techniques improves the mobility of the cervix and scar tissue.
Bladder pain syndrome: Releasing the tension in pelvic floor muscles and posture correction helps to reduce your symptoms. Incontinence can be treated with pelvic floor muscle training, positioning and certain stretches of the muscles in the pelvic floor area.
Vaginismus: Treatment involves stretching of pelvic floor tissues with external and internal techniques, scar mobilization, muscle overactivity with dilators and relaxation techniques.
Dysmenorrhea: Techniques involve breaking the adhesions in the pelvic floor area and release the narrowing in the cervix.
Techniques to help to reduce your pain:
- Relaxation techniques,
- stretches,
- soft tissue release
Injury with any activity:
Pudendal neuralgia: Your Physio will treat you with nerve release, stretches, and posture correction. Sensory re-education to reduce the numbness in the pudendal nerve supply.
Coccyx pain: Treatment involves pelvic floor relaxation techniques, mobilization of coccyx. We will mobilize it internally and externally. Proper positioning with cushion, exercises to improve the mobility helps to reduce the pain the coccyx.
Male pelvic pain: Treatment includes release of pelvic floor muscles to ease up the pain. We will treat you with stretches, positioning, mobilization, relaxation.
DON’T WAIT TO START PHYSIOTHERAPY TREATMENT
If you notice any of the above symptoms, it’s important to consult your pelvic floor physiotherapist. You can reduce the risk of complications by taking early treatment.. Book a consultation at PhysioNOW with a Registered Physiotherapist today.