What is a scaphoid fracture?
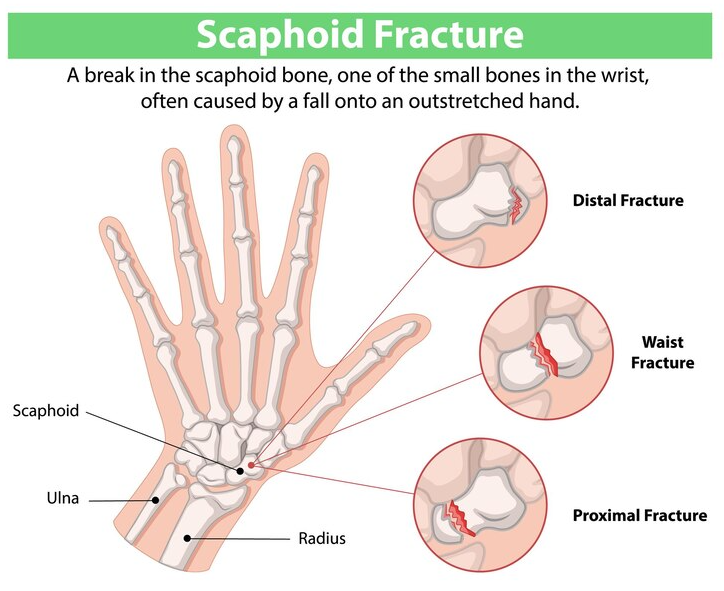
A scaphoid fracture is one of the most common types of wrist fractures, particularly among young adults and athletes. The scaphoid bone is one of the eight small bones in the wrist, located in the middle of the joint closer to the thumb side. Functionally, it helps to connect the forearm bones (radius and ulna) to the hand bones (metacarpals). A fracture of the scaphoid typically occurs when an individual falls onto an outstretched hand (commonly shortened to FOOSH), causing the wrist to bend backward in an awkward position. The impact can break the bone, leading to pain, swelling, and difficulty moving the wrist. Unfortunately, due to its location and blood supply, scaphoid fractures can be tricky to diagnose and treat, and failure to do so properly may lead to long-term complications.
How do scaphoid fractures happen?

The primary cause of a scaphoid fracture is trauma to the wrist, often from falling onto an outstretched hand. Some common scenarios include:
- Sports injuries: Athletes in contact sports such as football, basketball, or acrobatic sports like gymnastics are particularly prone to wrist injuries
- Motor vehicle accidents: Sudden impacts can cause severe trauma to the wrist, leading to fractures
- Repetitive stress: In some cases, repeated stress or pressure on the wrist may contribute to stress fractures of the scaphoid bone
Additionally, certain risk factors can make someone more prone to a scaphoid fracture, including:
- Age: Young adults, especially those between 18-30 years old, are more likely to experience this type of fracture
- Bone density: People with low bone density or osteoporosis may be more susceptible
- Activity level: Individuals involved in high-impact or contact sports have a higher risk of injury
What are the symptoms of a scaphoid fracture?
A scaphoid fracture is often difficult to diagnose at first because symptoms may resemble those of other wrist injuries. Common symptoms include:
- Pain in the wrist: The pain is usually felt on the thumb side of the wrist and may be more intense when the wrist is moved or when pressure is applied to the area
- Swelling and bruising: Swelling is typically visible around the base of the thumb, and bruising may appear later
- Reduced range of motion: It may be difficult to move the wrist or thumb without sharp pain
- Tenderness: Pressing on the area near the base of the thumb is very sore
How can this type of fracture be diagnosed?
To diagnose a scaphoid fracture, doctors will typically perform a physical examination and review the patient’s medical history, including any recent falls or trauma. X-rays are the primary imaging tool used to diagnose a scaphoid fracture, but it’s important to note that fractures may not always be visible immediately after the injury. Sometimes, a second set of X-rays taken a week or two after the injury is required to detect any changes. Unfortunately, scaphoid fractures are unique, and some may never be detectable on x-rays, called occult scaphoid fractures. In these cases, the physical exam and symptoms can usually inform the diagnosis of a fracture.
How is a scaphoid fracture treated?
Treatment for a scaphoid fracture depends on the severity of the break and its location. Generally, treatment options include:
- Conservative treatment: Non-displaced fractures (where the bone fragments remain in alignment) are often treated with immobilization using a cast or a splint. This method is typically effective for stable fractures, and the cast is worn for about 6-12 weeks. Here, the wrist is kept in a position that limits movement to allow the bone to heal properly
- Surgical treatment: Displaced fractures (where the bone fragments are out of alignment) often require surgical intervention. Typically, surgery involves realigning the bones and using screws, pins, or plates to hold the fragments in place during healing. Also, surgery may be necessary if there’s a concern about the blood supply to the scaphoid bone, which can be disrupted by a fracture. This is an important complication to watch for as it can lead to a serious issue if untreated, called avascular necrosis (AVN)
- Rehabilitation: After the cast or surgical treatment, physical therapy is recommended to help restore the wrist’s strength and range of motion. For example, rehabilitation exercises can aid in reducing stiffness, improving flexibility and function of your wrist and hand
Initially, range of motion exercises after immobilization should focus on active-assisted ROM as the hand and wrist will be stiff. These exercises should focus on the wrist and thumb; however, the fingers, elbow and shoulder also need to be considered as they may be affected. If the full range is still restricted, manual therapy can be applied in the form of joint mobilizations to the radio-carpal joint, radio-ulnar and carpal joints. Furthermore,, other forms of manual therapy may also be helpful to reduce any residual swelling or pain such as soft tissue work or massage techniques.
What can go wrong with a fracture?
Although most scaphoid fractures heal successfully with proper treatment, complications can arise. For example, some potential complications include:
- Nonunion: If the fracture does not heal properly, the bone may fail to unite, leading to chronic pain and dysfunction
- Avascular necrosis (AVN): The scaphoid bone has a relatively poor blood supply, and fractures, especially those in the proximal part of the bone, can disrupt blood flow. Consequently, this can lead to the death of the bone tissue, which may result in permanent wrist damage
- Osteoarthritis: Chronic wrist pain or deformity following a scaphoid fracture increases the risk of developing arthritis in the joint
How can I minimize the risk of a fracture?
While some scaphoid fractures are due to accidents or unavoidable trauma, there are steps you can take to reduce your risk:
- Wear protective gear: When engaging in sports or high-risk activities, wearing wrist guards or other protective equipment can reduce the chances of injury
- Strengthen the wrist: Regularly performing exercises that strengthen the muscles and ligaments around the wrist can provide more stability and help prevent injuries
- Fall prevention: Practicing good techniques and safety measures to avoid falling, such as using proper footwear can be especially beneficial
Looking for help?
If you are dealing with a wrist pain, post-fracture issues, or any other type if injury, look for PhysioNow! We have many experienced Registered Physiotherapists ready to help you get better! With 10 different clinics across the GTA from Burlington, Oakville, Mississauga and Etobicoke, our offices are in prime locations to serve you. Contact us if you have any questions and book with us today for your first assessment and treatment.