Now that the hottest days are behind us, running outdoors is possible again. If you’re a runner, whether casual or marathoner, your feet are your most valuable training partners. Namely, they take the full impact of every stride, supporting several times your body weight with each step. But when your feet start to ache or feel tight, it can throw off your training and may be the precursor to an injury. The good news? With a few smart habits and guidance from a physiotherapist at PhysioNow, you can keep your feet ready to go the distance. Find out how to do foot care for runners!
Why does foot care for runners matter?
Running is repetitive and high impact by nature. Unfortunately, repetitive tasks are where our bodies tend to struggle. Over time, even small imbalances in running gait, strength, flexibility, or footwear can build up stress on the feet and ankles. For example, if you’ve ever noticed one side of your shoe wears out faster than the other, that’s a sign that you have an imbalance in your weight distribution. While this imbalance does not guarantee an issue, it certainly increases your risk for it. Healthy feet help you absorb shock more efficiently, maintain good running mechanics, and prevent compensations that can have a chain reaction that causes issues in the knees, hips, or back.
What kind of foot issues do runners have?
While not exhaustive, these are some of the problems we see most often in the PhysioNow clinic:
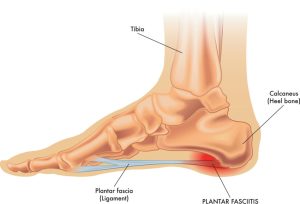
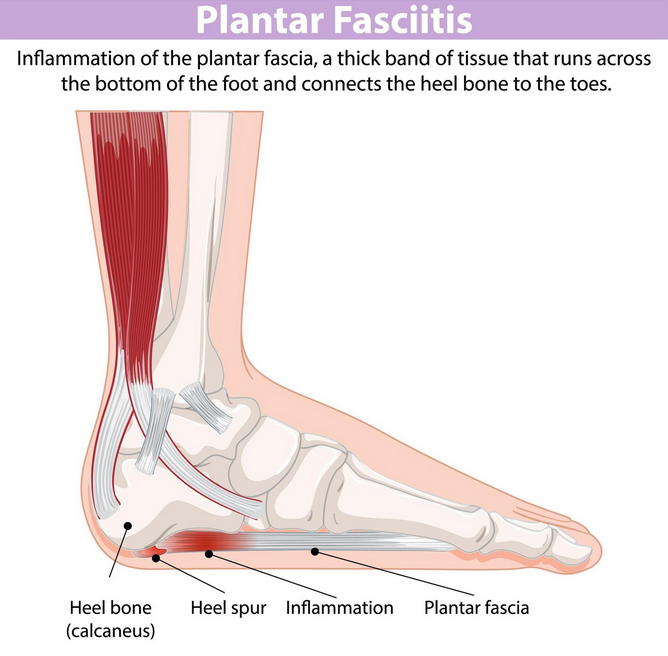
- Plantar fasciitis: Sharp heel pain that’s often worse first thing in the morning and the first couple of steps
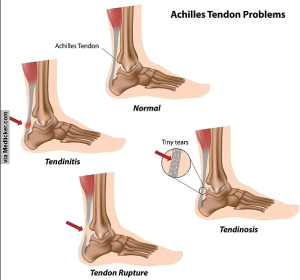
- Achilles tendonitis: Irritation and pain in the tendon connecting your calf to your heel
- Blisters or calluses: Usually caused by friction or poorly fitting shoes
- Stress fractures: Tiny cracks in foot bones from repetitive overuse
- Shin splints: Often linked to weak foot muscles or improper footwear
It is important to note that issues are not limited to the feet either. It is a 2 way street and the rest of the body may be causing a foot pain, or vice versa. This is often why it’s important to see a health care professional when treating these injuries. You want to treat the root cause, not just the symptoms.
What does foot care for runners look like?
1. Choosing the right shoes
Your running shoes should match your foot type, gait, and mileage. A gait assessment from a physiotherapist or running specialist can help determine whether you need neutral shoes, stability support, or even custom orthotics. Read our other blog to find out more about the benefits of custom orthotics! Recommendations are to replace your shoes every after 600km to avoid worn-out cushioning. Another tip is to alternate between a couple pairs of shoes to extend the lifespan.
2. Warming up and cooling down

Don’t skip mobility and flexibility work! Often the most neglected part of a workout, gentle calf stretches, ankle circles, and a few minutes of dynamic movement before and/or after you run can help your feet handle impact better. Rolling the soles of your feet over a ball or frozen water bottle can also relieve tightness after a run.
3. Strengthening your feet and body
Strong feet are shock-absorbing feet. Here are some foot care exercises we use commonly in the clinic.
- Towel scrunches: Use your toes to pull a towel toward you. Helps to strengthen intrinsic foot muscles
- Single-leg balance: Stand on one foot for 30 seconds to train stability. You can make this harder by balancing on different types of surfaces
- Heel raises: Build calf and arch strength. Progress by doing single leg heel raises
A physiotherapist can build you a progressive program that fits your training load. Remember that running is a whole body exercise and cross-training with resistance exercises and other forms of cardio is key. It is not enough to just be strong at the feet, your knees, core, hips and back are all contributing greatly during a run.
4. Listening to early signs of pain
A little muscle soreness is normal, but consistent pain, especially in the heel, arch, or top of the foot, isn’t. Addressing it early with physiotherapy can prevent a minor irritation from turning into an overuse injury.
5. Maintaining your feet
Basic foot care is a must! Keep your toenails trimmed, inspect your feet regularly for blisters or swelling, and use moisture-wicking socks to reduce friction. Pedicures are not just for looking good, they play a huge role in foot health as well can can help you manage rough spots on your feet. For more serious issues though, you should see a medical professional.
When should I see a professional?
If you’re noticing persistent foot pain, reduced performance, or recurring injuries, a physiotherapist or chiropodist can help. At PhysioNow, we have expert clinicians trained to assess gait, and that can also fit you for custom orthotics. Whether it’s a muscle imbalance, footwear issues, or running mechanics, we’ve got you covered. With hands-on treatment and a personalized exercise plan, you can get back to running comfortably and safely. PhysioNow has 10 locations across the west GTA including Burlington, Oakville, Mississauga, and Etobicoke. Book with PhysioNow today for your first assessment and treatment!