Prostatitis
Prostatitis or Prostatodynia Physiotherapy
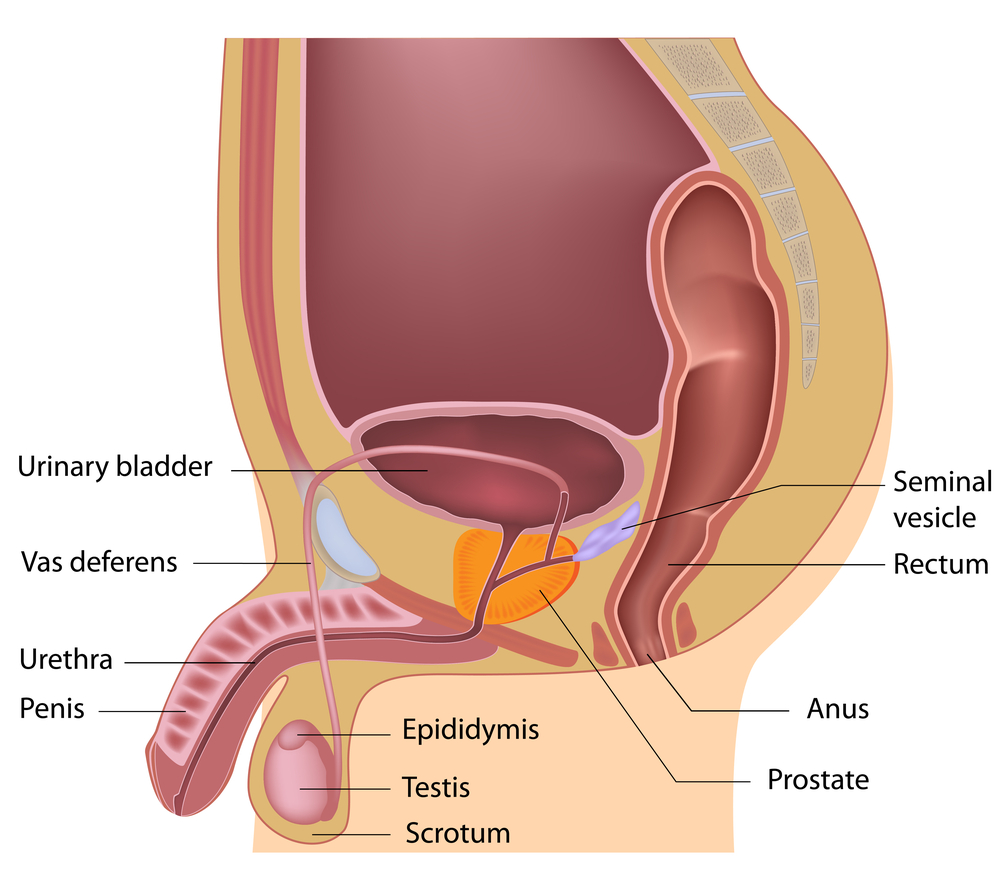
Prostatodynia or Chronic Pelvic Pain Syndrome (CPPS) is a pelvic pain condition in men. This means ‘inflammation of the prostate’. There are two basic types of prostatitis, acute and chronic.
Acute Bacterial Prostatitis
Acute Bacterial Prostatitis is an infection of the prostate. This type of Prostatitis causes chills and fever. In this case, you need your Doctor’s attention promptly!
Nonbacterial or Chronic Prostatitis
The other is Nonbacterial or Chronic Prostatitis. This can be treated with alternative treatments such as Pelvic physiotherapy, exercises, lifestyle modifications etc. Investigations in this case show that bacteria and yeast are negative. The physical examination does not usually show anything unusual. However, the prostate may be swollen. What can make the problem even more confusing is that often young, otherwise healthy men develop this condition. Antibiotics, pain-killers, and medications prescribed are often not effective. Many men have been told that they must learn to live with the symptoms because a cure is not available.
Symptoms may include a few or all of the following:
• Pain in the testicles, or tip, shaft or base of the penis
• Pain at the perineum (the area between the testicles and penis)
• Urination Causes Pain
• Increased pain in sitting
• Pain or discomfort with sexual arousal, or during or after ejaculation
• You May notice Pain or discomfort above the pubic bone
• Urinary frequency
• Urinary urgency
• Pain before, during or after a bowel movement
• Decreased interest in sex
Treatment
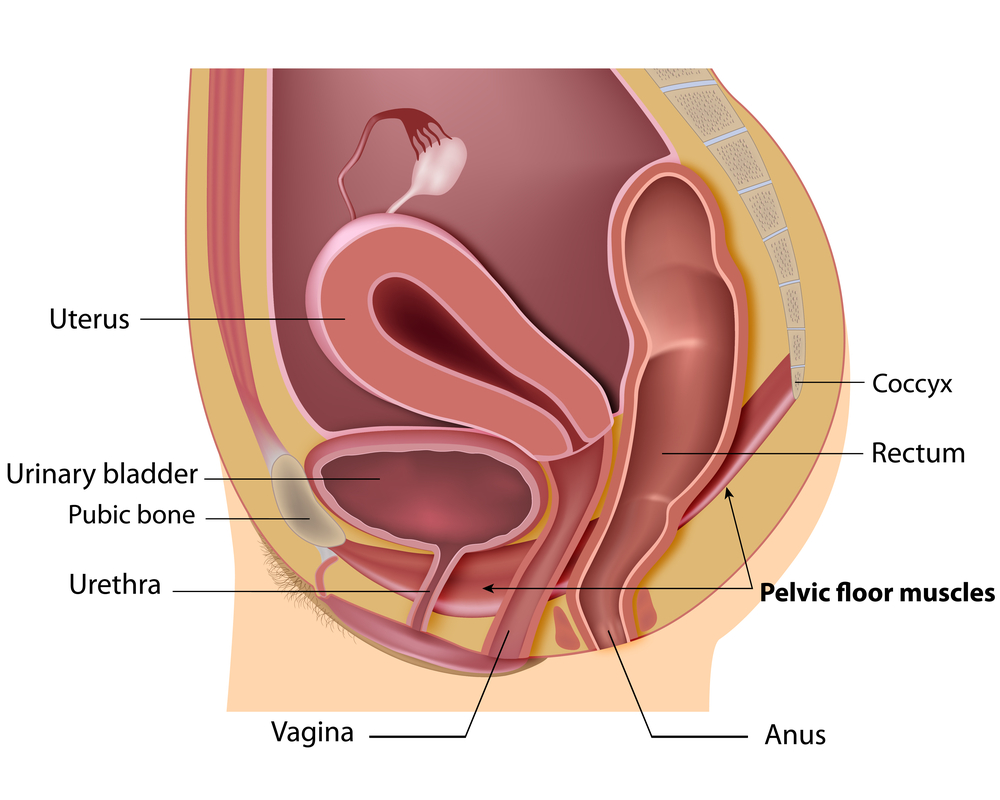
The Pelvic Health Physiotherapist creates an individualized treatment program. Treatment is based on pelvic floor dysfunction, symptoms, and response to the treatments.
The following treatment programs and techniques may be involved in Pelvic Physiotherapy for Prostatitis:
Trigger point release therapy
Trigger point release therapy is also known as myofascial trigger point release. Trigger point release therapy is an alternative treatment for chronic prostatitis. It is often helpful for treating CP/CPPS symptoms that are associated with stress and tension of the pelvic floor muscles.
Trigger point release therapy is often combined with paradoxical relaxation therapy. This exercise method involves autonomic self-regulation. This decreases pelvic floor muscle tension. It teaches you how to release this tension. Paradoxical relaxation involves a specific breathing technique to help relieve anxiety.
Total body
Total body (exercise, chronic stress management, lifestyle) changes help relieve pain. It is important to know which foods make the symptoms worse. Try to avoid those foods. The most common foods that have been found to trigger symptoms include:
• Spicy foods
• Hot peppers
• Alcoholic beverages
• Acidic foods
• Wheat
• Gluten
• Caffeine
Check out this patient’s experience.
Please call PhysioNow today to get started on your recovery from Prostatitis.

 Female & Male pelvic pain
Female & Male pelvic pain