
Pelvic Floor: Posture
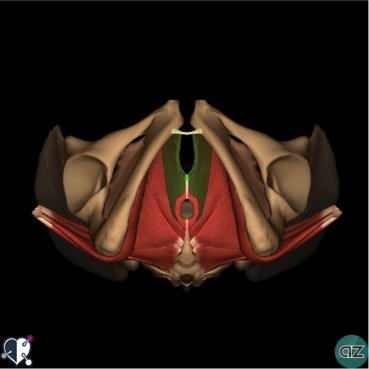
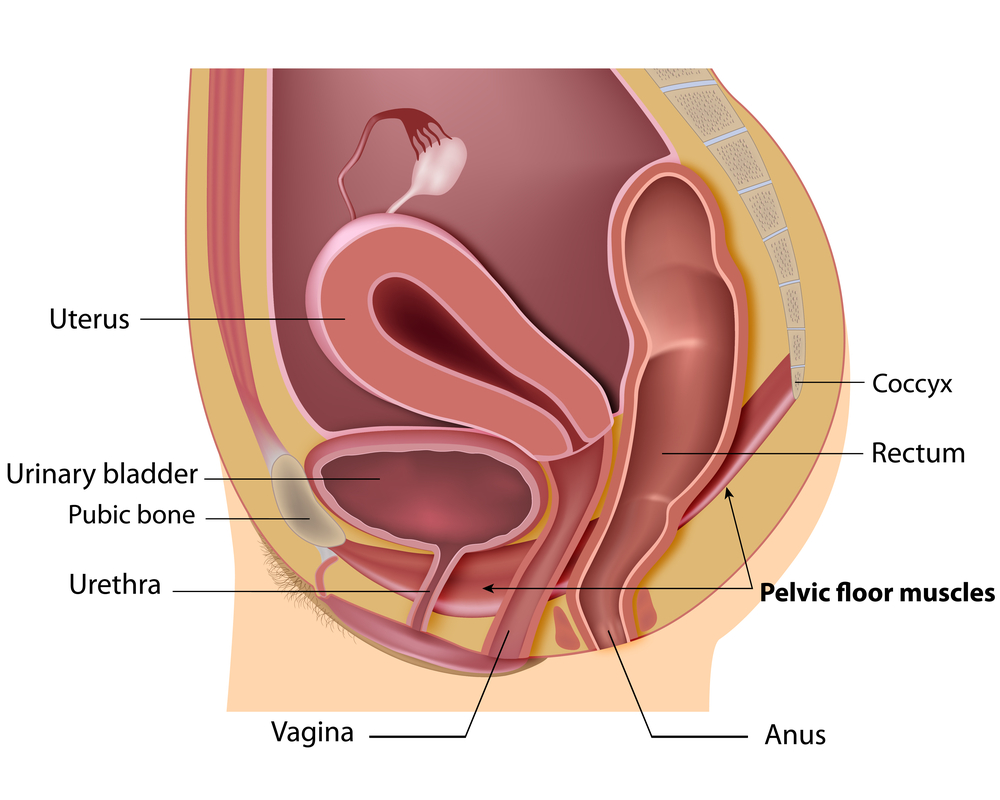
PELVIC FLOOR: POSTURE is a very important area if you have issues with urinary incontinence, pelvic pain, etc. The muscles of the pelvic floor support the abdominal and pelvic viscera. These muscles are active in standing and sitting. Furthermore, because the abdomen is a fluid-filled cavity, intra-abdominal pressure is distributed in all directions. The Pelvic Floor muscles, which form the floor of the abdominal cavity, contribute to its muscle control.
As a result of this contribution to control of intra-abdominal pressure, the muscles of the pelvic floor are likely to contribute to control of the spine and pelvis. The slouched posture places a lot of pressure on our internal organs and pelvic floor. This can cause a worsening of:
- urinary incontinence,
- pelvic pain,
- symptoms related to prolapse,
- and rectus diastasis.
Pelvic Floor: Posture, sitting slumped
- Research has shown that when we sit in a slumped posture, our pelvic floor muscle activity is much less than when we are sitting tall.
- Pelvic Floor: Posture IS VERY IMPORTANT!
- slouched sitting postures decrease the activity of your transverse abdominal muscles.
- A Proper breathing pattern encourages the pelvic floor to move more dynamically.
- Dysfunctional breathing patterns inhibit this dynamic movement of the pelvic floor.
Pelvic Floor: Posture,
- An assessment by a Pelvic Health Physiotherapist includes a thorough postural examination.
- Your Pelvic Health Physiotherapist will be able to identify your unique postural compensations
- They can help guide you on the road to improved body posture awareness.
CHECK OUT THIS LINK FOR FURTHER INFORMATION.
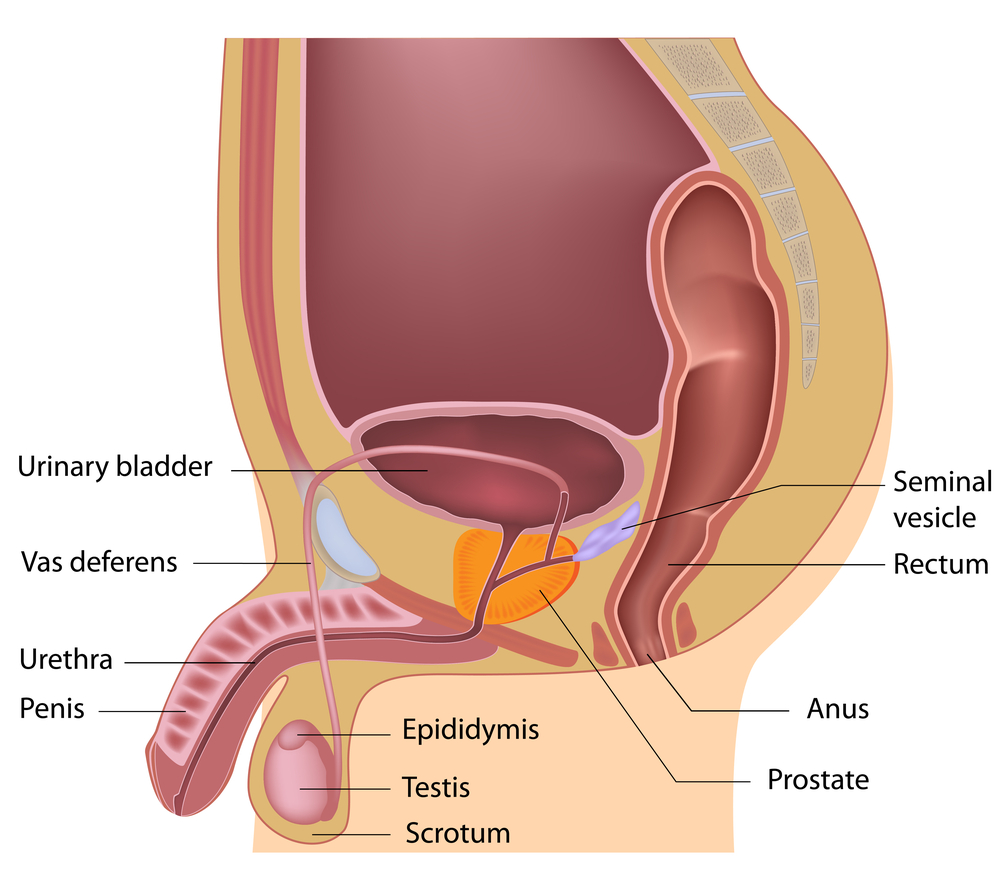
At PhysioNow, we have fully trained Pelvic Health Physiotherapists that can help to assess and treat pelvic issues like the following conditions:
- Constipation
- Dyspareunia
- Endometriosis
- leakage of urine
- pain with intercourse
- pelvic organ prolapse
- pelvic pain
- urinary incontinence
- vaginismus
- erectile dysfunction
If you or someone you know suffers from one of these conditions, give us a call today. We would be happy to help!
- Sapsford, RR. et al (2006) Sitting posture affects pelvic floor muscle activity in parous women: an observation study. Aust L Physiother. 52(3):219-22
- Reeve, A., Dilley, A., (2009) Effects of posture on the thickness of Transverse Abdominal Muscle and Pelvic Floor Muscle Exercises for Stress Urinary Incontinence: A Randomized controlled Trial. J Phys Ther Sci. 26(8): 1161-1163.






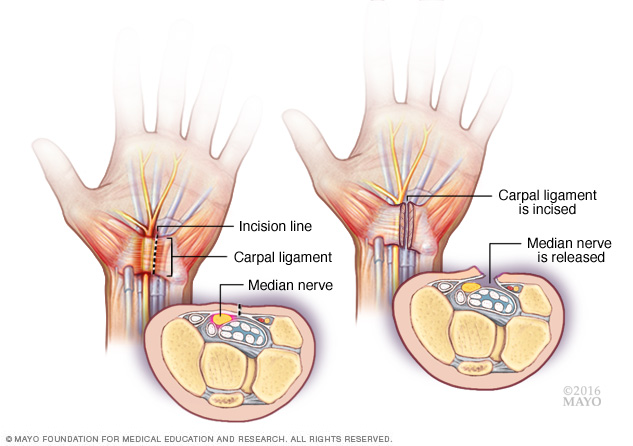 Resolution of the symptoms after surgery can be more temporary if the symptoms originate from elsewhere. Our experienced Registered Physiotherapists at PhysioNow will assess you to find out the actual cause of your symptoms and will help you to get rid of your symptoms. Call
Resolution of the symptoms after surgery can be more temporary if the symptoms originate from elsewhere. Our experienced Registered Physiotherapists at PhysioNow will assess you to find out the actual cause of your symptoms and will help you to get rid of your symptoms. Call