What is osteoporosis?

Osteoporosis is a disease that affects the bones of the body. It involves processes where the body is losing too much bone or is making too little bone. Additionally, it can also be a combination of both. As a result, the affected bones become weakened. Physiotherapy for osteoporosis is an important treatment tool to prevent fractures and improve a person’s quality of life.
How can osteoporosis impact a person’s life?
Normal and healthy bones can withstand a lot of stressors. However, osteoporotic bones, on the other hand, may break with just minor incidents. For example, a person with osteoporosis may fracture a bone from a simple fall or a minor bump. Furthermore, in very severe cases, just a sneeze may be enough to cause fractures to a bone.
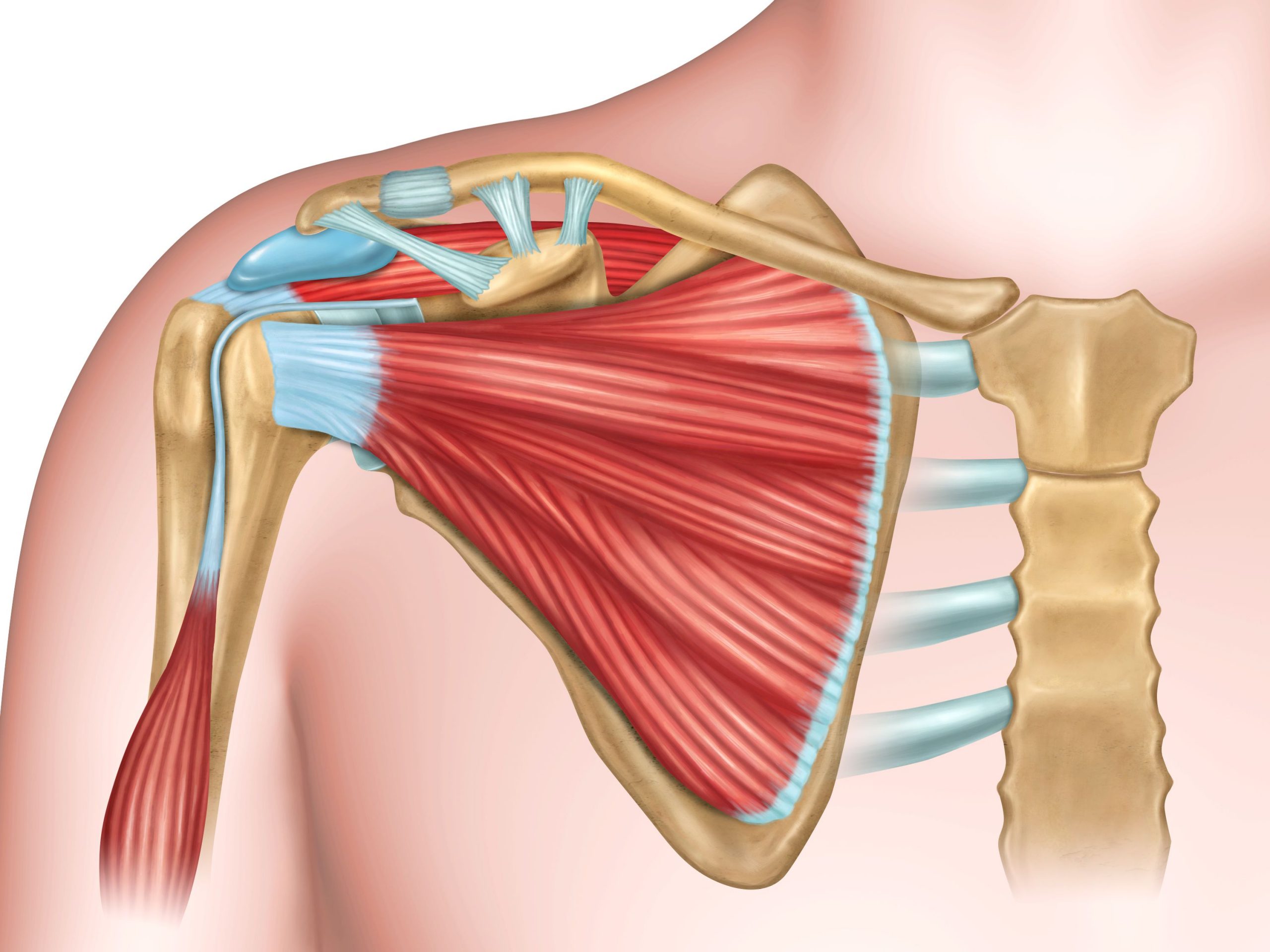
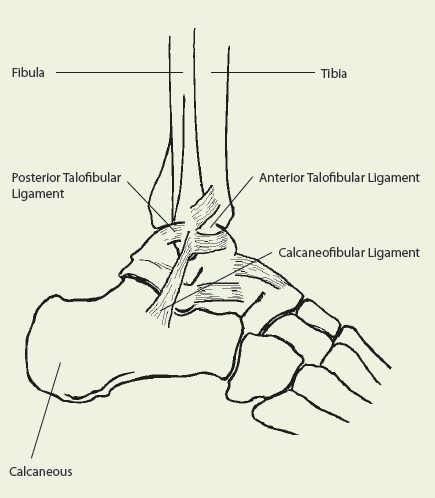
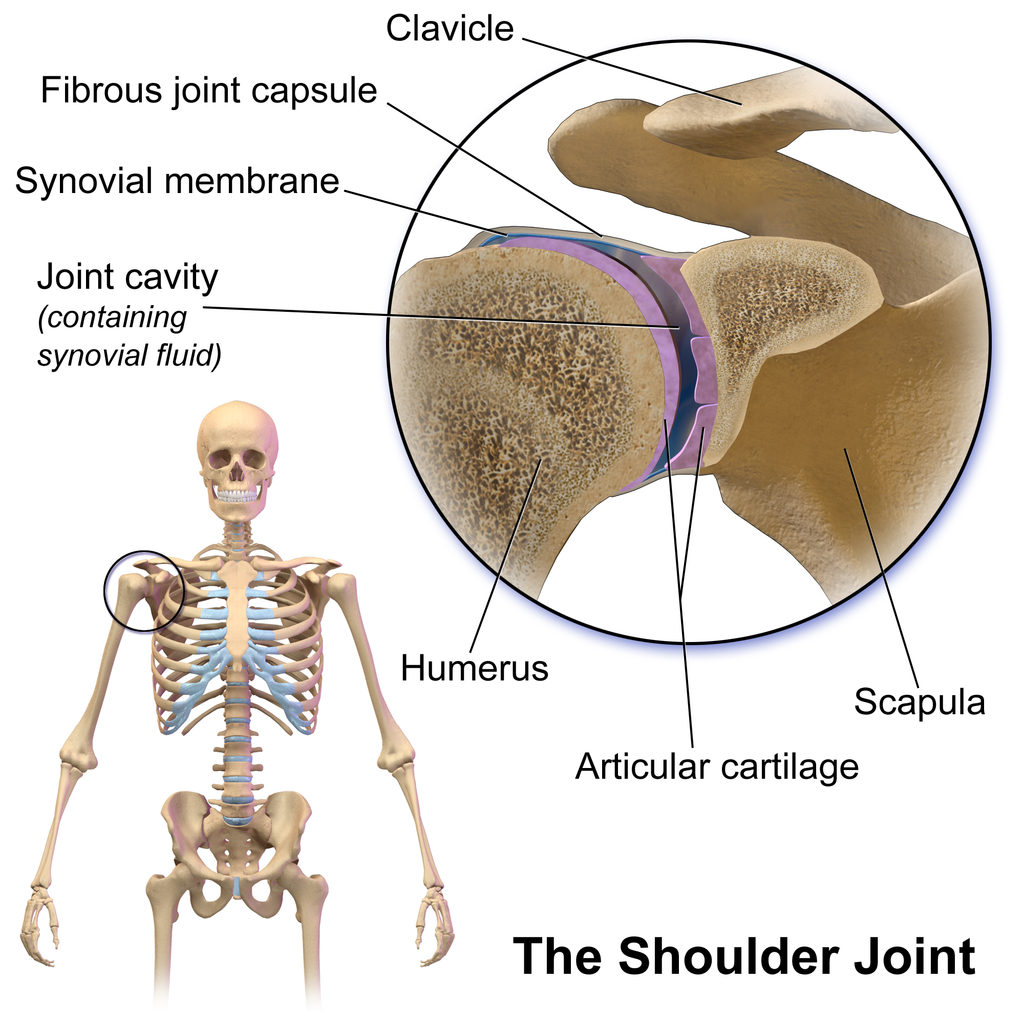
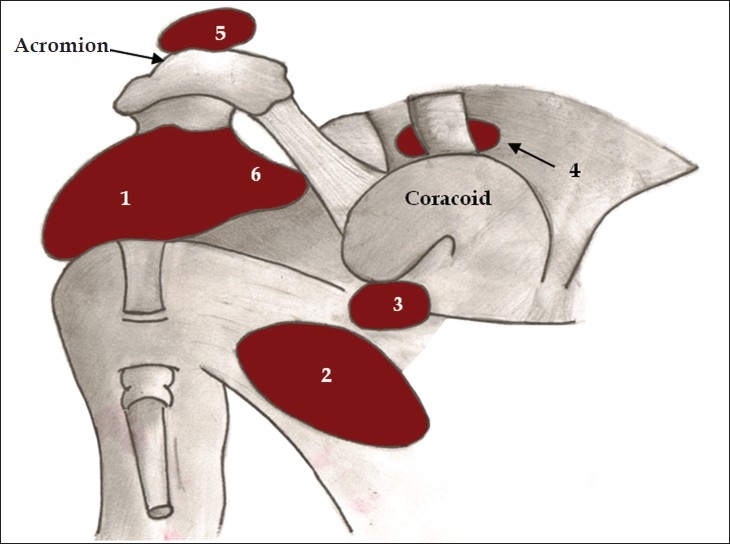
The term osteoporosis means “porous bone”, which refers to the look of the bone under a microscope. Normal or healthy bone looks like a honeycomb. However, with osteoporotic bones, the holes and spaces in the honeycomb are much bigger. This reflects the loss of bone density that occurs with the disease. These changes can happen over several years without any symptoms. However, by the time the affected bones break, the disease is usually more advanced. Consequently, the most common fractures associated with osteoporosis are in the hip, spine, wrist and shoulder.
What causes osteoporosis?
Osteoporosis does not have one specific cause. However, there are several potential risk factors for developing the disease. For example, some of these factors include:
- Age
- People can get osteoporosis at any age, but it tends to be rare under the age of 50
- Sex
- Compared to men, women are twice as likely to get osteoporosis
- Specifically, women also have an increased risk of bone mineral loss as they reach menopause as estrogen levels dramatically decrease
- Low body weight
- Small and thin people tend to break more bones
- This could be due to several factors including poor nutrition, low muscle mass, and low circulating estrogen
- Lower bone mineral density
- Having a parent who had a hip fracture
- Osteoporosis does have genetic component and tends to run in families
- A past history of broken bones
- People who break a bone as an adult may already have osteoporosis and not know it
- Some broken bones are obvious and others are hard to detect
- Vertebral factures can be painless, but each broken vertebra raises the risk for another
- These fractures may not be discovered until a person has developed an extreme curvature of the spine
The risk factors described above are inherent to the person. This means that they cannot be changed.
Changeable risk factors for osteoporosis
- Not getting enough calcium and vitamin D
- Calcium drives all our bodily processes, including those of bone health
- To absorb the calcium from our foods, we need to have vitamin D
- Not eating enough fruits and vegetables
- Calcium and vitamin D are only two of the nutrients important for bones
- We also need magnesium, potassium, vitamin K and others which we can get from eating a diet rich in fruits and vegetables
- Not getting enough exercise
- Bones require the push of gravity and the pull of muscles to maintain its strength
- Therefore, bone mineral and muscle mass are lost at an increased rate when there isn’t enough physical activity
- This is especially important for those over 50 years of age
- Drinking too much
- Heavy drinking makes bone weaker and easier to break
- More specifically, heavy drinking means more than 2 alcoholic beverages a day for women and three a day for men
- Dieting too much
- Very rapid weight loss causes bone loss by ‘unloading’ the skeleton
- Some fad diets can result in avoiding some nutrients, which can pull minerals from bones
- Smoking
- Smoking can cause skeletal damage and increase the risk of fractures
What is secondary osteoporosis?
Secondary Osteoporosis is when bone density loss occurs from having another disease or condition or from the treatment of another condition. More specifically, some medical conditions that can cause bone loss, falls and/or fractures include:
- Rheumatoid arthritis and other rheumatological conditions
- Malabsorption syndromes
- Sex hormone deficiency
- Primary hyperparathyroidism
- Chronic kidney disease
- Chronic liver disease
- Diabetes
- Chronic obstructive pulmonary disease (COPD)
- Neurological disorders
Additionally, some medications that can cause bone loss, falls and/or fractures include:
- Synthetic glucocorticoids (eg. Prednisone)
- Breast cancer drugs
- Prostate cancer drugs
- Excessive thyroid hormone replacement
- Anti-seizure and mood-altering drugs
- Blood pressure medication
- Diuretics
How do we diagnose osteoporosis?
Doctors diagnose osteoporosis using Bone Mineral Density (BMD) tests. Specifically, these tests measure the density of the bones and can accurately indicate whether an individual has osteoporosis. Additionally, a BMD test can also tell you how likely you are to develop osteoporosis in the future. Moreover, this information is so vital to prevent fractures and further bone loss.
A great resource for learning more about osteoporosis is through the Osteoporosis Canada website.
Can physiotherapy for osteoporosis help?
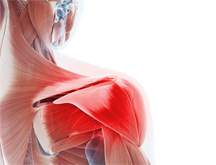
Physiotherapy can definitely help those affected by osteoporosis. Unfortunately, there is no cure for osteoporosis and it is a condition that needs management for the rest of a person’s life. Registered Physiotherapists are movement and exercise specialists and exercise is an important component for the management of osteoporosis. More specifically, poor posture, combined with the loss of bone density, can increase the risk of spinal fractures. Therefore, exercises can help strengthen the muscles responsible for posture and will help reduce the fracture risk.
Most importantly, physiotherapists can help design an individualized exercise program that targets the specific needs of a patient. Moreover, the physiotherapist can also provide important education to the patient to help keep them motivated and committed to their program.
What type of exercises should be included in a physiotherapy for osteoporosis program?

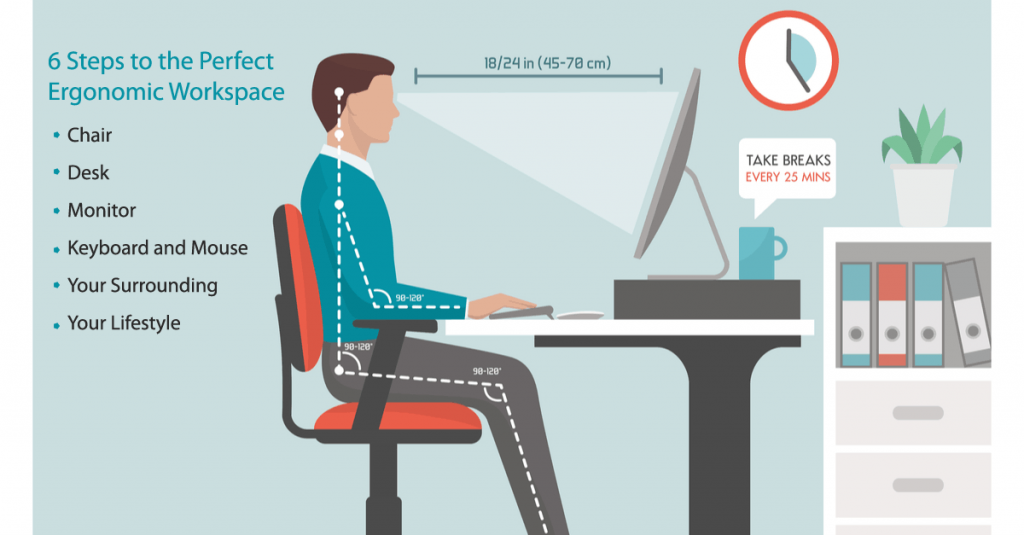
A good exercise program for individuals who have osteoporosis should include several different components. Specifically, the 4 main aspects of the program should include:
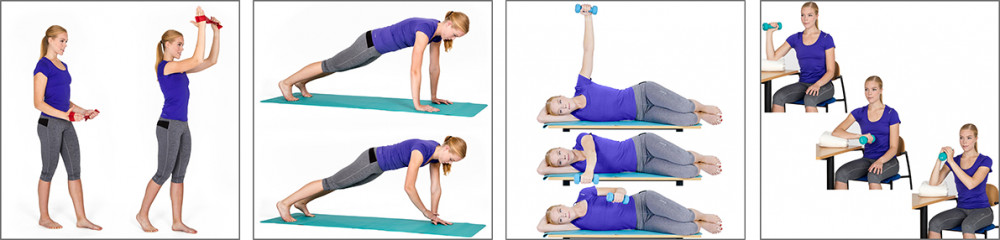
- Strength training
- Exercises that target the legs, arms, chest, shoulders and back
- Resistance can start with body weight and progress to moderate weights if it’s deemed safe
- Strength training should be completed twice a week
- Balance exercises
- Exercises that stress the balance system of the body in various ways to help strengthen it
- Exercises can include weight shifting, single leg standing and working on uneven surfaces
- Balance exercise need to be completed every day
- Posture awareness exercises
- The physiotherapist will explain what optimal posture is and help correct the patient’s existing posture
- Postural awareness should be practiced every day
- Aerobic Exercises
- Aerobic exercises should be completed in increments of 10 minutes or more
- The intensity should be between moderate to vigorous
- It is recommended that at least 150 mins/week of aerobic activity is completed
Consequently, physiotherapy for osteoporosis can be a major part of the management for this condition. More specifically, for a person just starting out with an activity program after receiving an osteoporosis diagnosis, the guidance of a registered physiotherapist can be very important. For example, the physiotherapist will help set some goals and ensure that safe exercises are chosen as part of the treatment plan. Therefore, as the individual feels more comfortable and starts to build some strength, the physiotherapist can also help progress the exercises as necessary. All in all, physiotherapy for osteoporosis is an integral part of osteoporosis management.
Call PhysioNow today to book your assessment with a Registered Physiotherapist.