Medical terminology can be a patient’s biggest nightmare. During a session, a lot of unfamiliar terms describing symptoms, conditions, muscles, and more can be used. Today, we will be discussing a process called centralization and peripheralization that is encountered a lot during physiotherapy. To elaborate, spinal and musculoskeletal pain and other symptoms can sometimes move, change location, or feel different with certain movements or exercises. The two important terms physiotherapists use to describe these changes are centralization and peripheralization.
Understanding these concepts helps you understand your treatment, reduce fear, and improve your rehabilitation outcomes.
What is centralization?
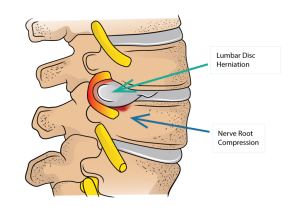
Centralization occurs when pain that was felt farther away from the spine (for example, in the leg or arm) moves closer to the spine or reduces in intensity with specific movements or positions.
Examples of centralization include:
- Leg pain moving from the calf to the thigh
- Arm pain reducing and becoming more localized to the neck
- Radiating pain decreasing while central discomfort remains
Centralization is generally considered a positive sign in physiotherapy.
What is peripheralization?
Peripheralization is the opposite phenomenon. It occurs when pain:
- Moves farther away from the spine
- Becomes more widespread
- Increases in intensity in the limb
For example:
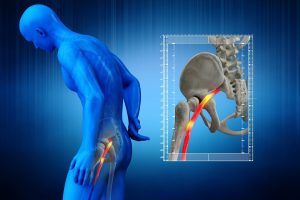
- Low back pain spreading further down the leg
- Neck pain traveling into the arm or hand
- Symptoms becoming sharper or more intense at areas farther from the spine
Peripheralization often indicates that a movement or load is not currently well tolerated.
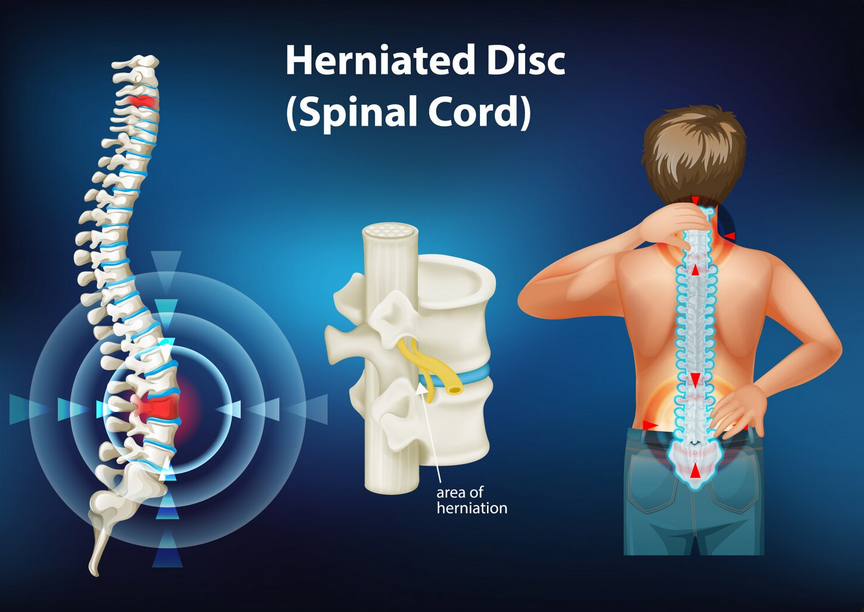
Why do centralization and peripheralization occur?

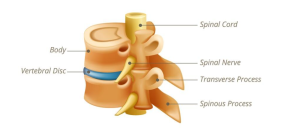
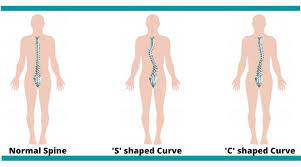
The spine, discs, joints, and nervous system are highly interconnected. Changes in symptoms reflect how these systems respond to movement and load.
Possible contributors include:
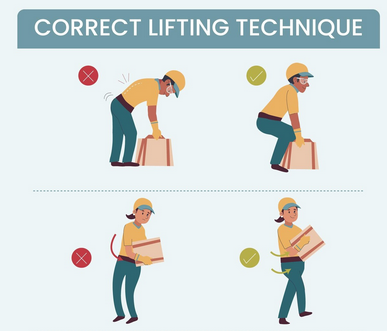
- Mechanical loading of spinal structures
- Sensitivity of neural tissues
- Protective responses from the nervous system
- Individual movement patterns and postures
Ultimately, these symptom changes provide valuable information for guiding treatment. Your physiotherapist can interpret these changes to determine whether the treatment is working well, or whether a different technique needs to be used.
Why is centralization important for physiotherapy?
A condition that displays centralization is commonly associated with:
- Improved outcomes
- Reduced nerve irritation
- Better tolerance to movement
When symptoms centralize, physiotherapists often continue or build upon the movements that produce this response. So what happens to the patients that don’t show a centralization response? Unfortunately, while centralization is desireable to have, not all patients experience it. Thankfully, many people still recover fully without clear centralization patterns, it just may take more time.
Physiotherapy always considers the whole clinical picture, including function, pain levels, strength, and confidence with movement.
What does peripheralization mean for treatment?
Peripheralization does not mean lasting harm or damage is being done to the tissue. Instead, it signals that:
- A movement may need modification
- Load may need to be reduced
- A different strategy may be more appropriate
Physiotherapists use this information to adjust treatment safely and effectively. A movement that causes peripheralization may become a part of treatment later on, but is currently not appropriate.
A summary of centralization vs peripheralization

Physiotherapists assess symptom responses during:
- Repeated movements
- Postural changes
- Functional tasks
This helps identify patterns of centralization vs peripherilization:
- Movements that reduce symptoms
- Movements that aggravate symptoms
- Optimal starting points for rehabilitation
Treatment is then tailored to encourage positive responses while avoiding unnecessary symptom flare-ups.It’s important to understand that symptom location does not always reflect tissue damage where the pain is felt. Even though your pain might be in the ankle, your physiotherapist will be checking your back for the possibility of referred pain.
Looking for physiotherapy treatment?
Look for PhysioNow! We have 10 locations across the west GTA including Burlington, Oakville, Mississauga and Etobicoke. Our expert clinicians can help you recover from an injury, neck pain, back pain, and more. Don’t wait any longer, we can help you get back to your normal life. Book with PhysioNow today for your first assessment and treatment. We can be reached at P: 289-724-0448 Email: applewood@physionow.ca