Shoulder Pain
Shoulder pain is a common problem for many people. It can happen to people of all ages from children to the elderly. The pain can be very severe and cause a lot of limitations with work and activity. Shoulder pain is one of the top 5 reasons why people seek out physiotherapy and massage treatments.
What Causes Shoulder Pain?
There are several reasons why people suffer from shoulder pain.
Trauma
Any type of direct or indirect trauma can produce shoulder pain if the arm and/or shoulder is involved

-
- Motor vehicle accidents
- Falls
- Sports injuries
- Violent incidents
Poor office ergonomics
Many people who work in offices spend majority of their time sitting in front of a computer for long periods of time. Additionally, many offices do not always provide optimal ergonomic setups for their staff. Over time, as a result, this may lead to the development of pain and stiffness in the shoulder.
Examples of poor ergonomics include:
-
- poor desk and screen height
- poor positioning of the keyboard and mouse
- inadequate chair height and support

Poor day to day posture
Shoulder pain related to posture usually develops over time with certain habits. For the most part, some of these habits we just adopt over time. For instance, examples include looking at our phones for long periods of time or spending hours playing video games. In other words, shoulder pain can develop from poor posture if we do not make an effort to be more active during our day.
Repetitive activities
Many people perform tasks that are repetitive at work and/or home. For instance, overhead lifting, sorting on an assembly line and typing are examples of repetitive activities. These repetitive activities can certainly take their toll if it has been going on for a long period of time. Therefore, if the shoulder is not strong enough to support the work that it’s having to do, then injury may occur.

Consequently, it is not uncommon for people who do a lot of repetitive manual labour to hurt their shoulder at work. In Ontario, if workplaces are registered with the WSIB or the Workplace Safety & Insurance Board, they may qualify to get physiotherapy treatment.
Congenital or Developmental changes
Some people are born with a unique bone structure that may place them at increased risk of injury. For example, if the acromion of the shoulder blade has a hooked shape, there is more potential for a rotator cuff injury. Similarly, your genetics may influence the shape of your bones in the shoulder. This may lead to an increased risk of shoulder pain as a result.
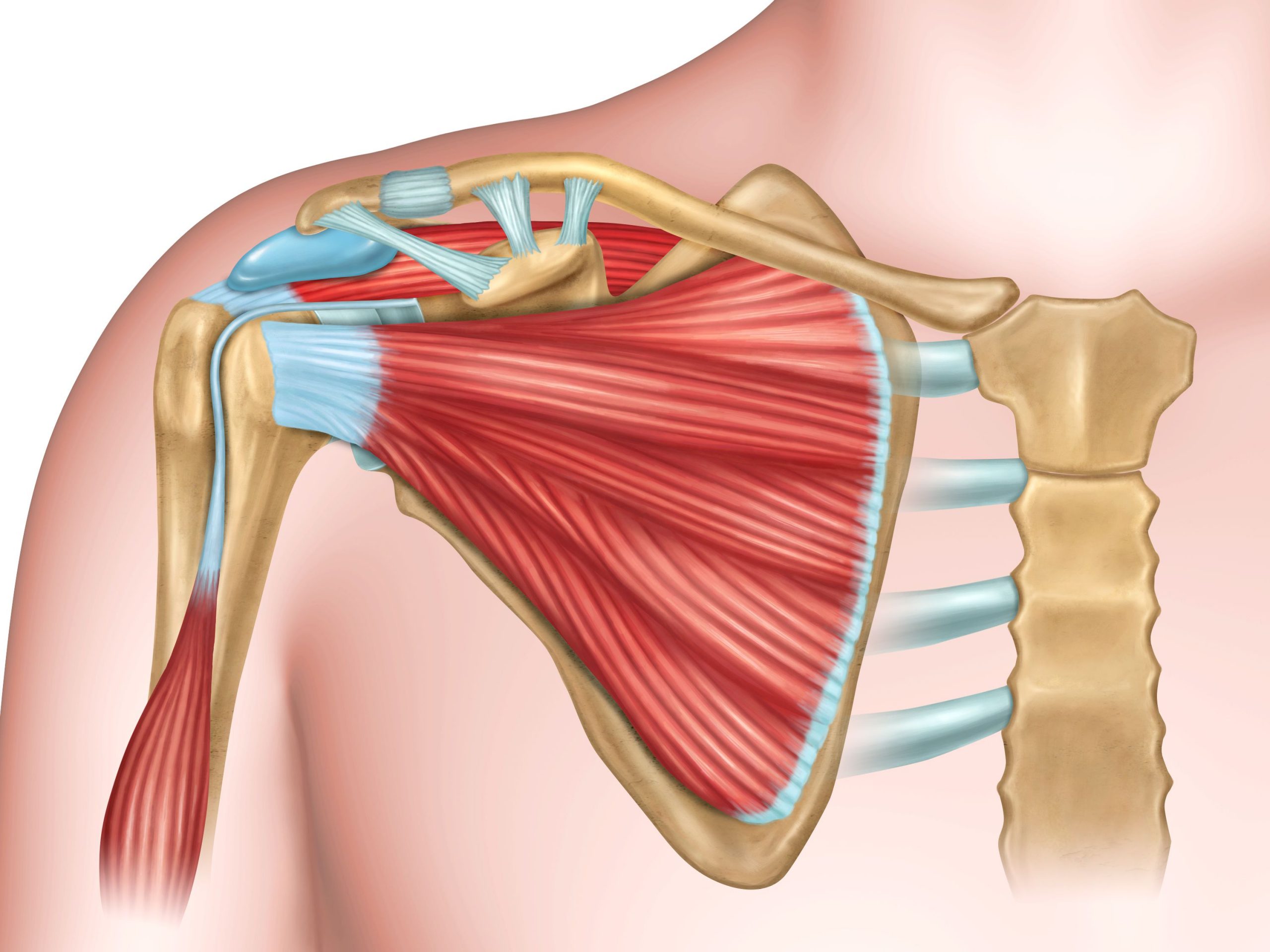
Some Basic Shoulder Anatomy
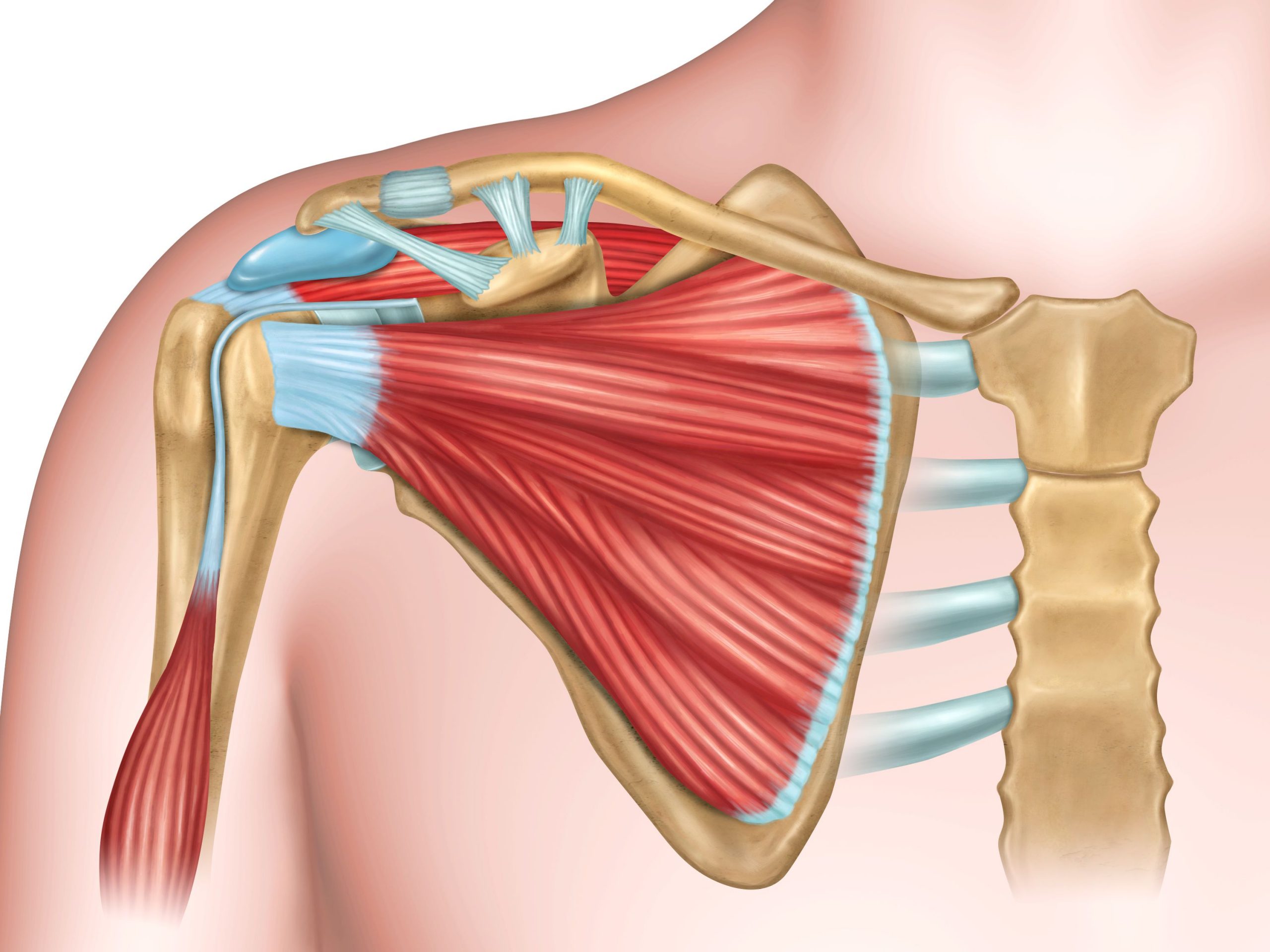
Having some knowledge of basic shoulder anatomy will help with understanding why shoulder pain develops. The shoulder joint is quite complex. Specifically, there are a lot of structures that attach to or present around the shoulder. For example, these structures include tendons, ligaments, bursae, cartilage and the joint capsule. Furthermore, the shoulder joint is held together by mostly soft tissues without a lot of bony protection. This setup specifically allows for a lot of movement. However, as a result there is less stability through the area.
What structures makes up the shoulder joint?
The shoulder is made of 4 separate joints that work together to allow function:
- Glenohumeral (GH) joint – this is a ball and socket joint and is where majority of our arm movement happens. The socket is made up by part of the shoulder blade and the ball is made up of the humerus, which is the long bone of the upper arm.
- Acromioclavicular (AC) joint – joint between the acromion of the shoulder blade and the collar bone.
- Sternoclavicular (SC) joint – joint between chest bone and the collar bone.
- Scapulothoracic joint – the joint between the shoulder blade and the ribs at the back of the chest.
Why is the shoulder joint prone to pain?
The shoulder is held together by many soft tissues including ligaments, muscles and tendons. Other important anatomical structures include the joint capsule surrounding the ball and socket joint and the subacromial and subdeltoid bursae. The function of the joint capsule is to protect the joint and produce a lubricating fluid. The bursae are small fluid-filled sacs that act as a cushion between the bone and other moving parts.
What are some of the injuries that can happen to the shoulder?
- Sprains/Strains of any of the muscles, tendons and ligaments
- Tears/Ruptures of any of the muscles, tendons and ligaments
- Tendonitis/Tendinosis
- Fractures
- Bursitis
- Dislocations
- Adhesive Capsulitis or Frozen Shoulder
- Osteoarthritis
- Nerve entrapments/injuries
Signs and Symptoms of Shoulder Injuries
- Pain
- Swelling
- Restricted range of motion
- Weakness
- Instability
- Bony deformities
Healing Times for Shoulder Injuries
The healing time for shoulder injuries will vary depending on the injury. Most simple sprains and strains will take anywhere from 6-8 weeks to get better. On the other hand, other types of injuries may need more time to recover. For example, muscle or tendon tears can take 6-12 months to improve. And similarly, frozen shoulders can take well over 1 year to improve. Therefore, the timeline for healing really depends on the nature of the injury. Additionally, there are a lot of individual differences in healing time even for similar injuries. Some of these factors include:
- Age
- Level of fitness and/or mobility
- Commitment to treatment
- Consistency of doing home exercise program
- Ability to modify workplace or home environment to allow for optimal treatment response
- Presence of other injuries
- Amount of time that they injury/pain has been present
Treatment for Shoulder Pain
The treatment for shoulder pain will depend on the type of injury and the structure(s) that has been injured. Most importantly, it is important to understand that the shoulder is made up of 4 different joints. Additionally, these 4 joints are all interconnected with each other. Therefore, treatments needs to target the whole shoulder complex and not just the individual structures involved. Consequently, this will allow the shoulder to return to its full potential and reduce the risk of re-injury.
The main goals of any shoulder pain treatment will be to:
- Reduce pain
- Regain full range of motion
- Regain strength and stability
- Return to pre-injury activities
What is the typical treatment for shoulder pain?
Treatment for shoulder pain usually has multiple components. The Registered Physiotherapist will start with a thorough assessment. Firstly, this allows them to identify the source of the shoulder pain. Secondly, based on the assessment, the physiotherapist is able to provide the most appropriate treatment. Specifically, examples of physiotherapy treatment can typically include:
- Manual therapy
- soft tissue work
- mobilizations
- assisted stretching of the shoulder and associated areas

- Modalities – these are usually used in the acute phase for pain relief
- Ultrasound
- Laser
- IFC or TENS
- Acupuncture
- Heat/Ice
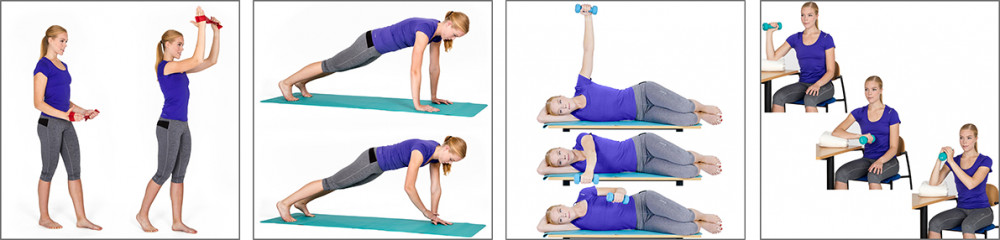
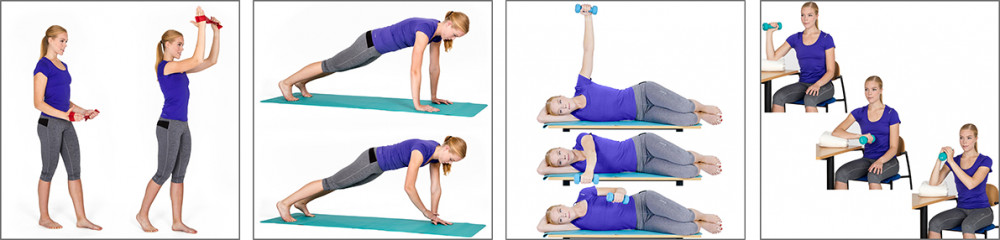
- Exercises
- Range of motion and strengthening exercises that are specific to the injury
- It is important that the patient completes the prescribed exercises on a regular basis at home. Firstly, this allows the patient to make the necessary changes with movement and strength. More importantly, however this allows the patient to be independent and provide self treatment on a daily basis.
- Education
- Explanation of the condition
- Rationale for the treatment choices
- Do’s and don’ts to help the injury along
In conclusion, shoulder pain can be quite debilitating for many people. Therefore, it is important to seek out a registered physiotherapist for assessment and treatment sooner than later. Similarly to most other injuries, the longer an injury is left untreated, the more chronic it becomes. Consequently, this makes it more difficult to resolve in a timely manner. Call PhysioNow today to get treatment for your shoulder injury. Our experienced physiotherapists and massage therapists in Mississauga, Etobicoke and Oakville will help you recover!
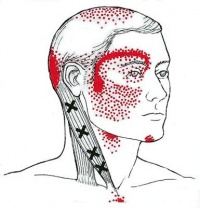
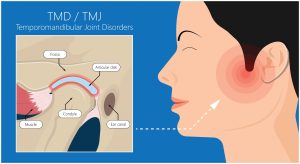 Headaches stemming from the jaw result from dysfunction in the jaw joint, anatomically known as the temporomandibular joint (TMJ). This joint connects your lower jaw to the skull and is used in actions such as talking and chewing as it allows the opening and closing of the mouth. Therefore, headaches are one of the common symptoms of jaw dysfunction. Though they are lesser known, it is commonly missed as a source.
Headaches stemming from the jaw result from dysfunction in the jaw joint, anatomically known as the temporomandibular joint (TMJ). This joint connects your lower jaw to the skull and is used in actions such as talking and chewing as it allows the opening and closing of the mouth. Therefore, headaches are one of the common symptoms of jaw dysfunction. Though they are lesser known, it is commonly missed as a source.