What’s the difference between leg extension and squats, and which ones better for you?
If you find are an avid gym goer yourself, you’ve probably heard some version of this argument. When discussing leg workouts, there is much debate surrounding the importance of leg extension versus squat movement. Although both of these exercises can be performed in a gym setting, they provide different results based on how each exercise incorporates various types of movement patterns into your workout regimen.
Breaking down leg extensions vs squats
Let’s begin with understanding the basis of these two exercises.


Leg extensions are a targeted movement for the quads (your big thigh muscles), providing an extremely isolated contraction. In this context, isolated means that the quads are the only muscles performing major work, the other muscles groups contributions are minimal. Consequently, the result is a complete and intense contraction of your quads at the end of each rep. If you want to develop a teardrop shape in your quad muscles, leg extensions are a great exercise to add to your routine.
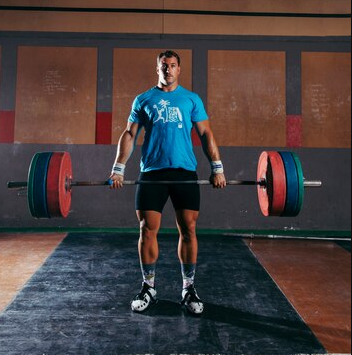
On the flip side, squats are the undisputed king of compound movements. They engage your entire lower body and core, making them the perfect exercise for building overall strength and functional fitness. Plus, squats are just plain awesome for building those glutes and hamstrings, in addition to quads. Because of this difference, leg extension and squat exercises cannot replace one another and serve different purposes in your leg training program.
Comparing the pros and cons of leg extensions vs squats
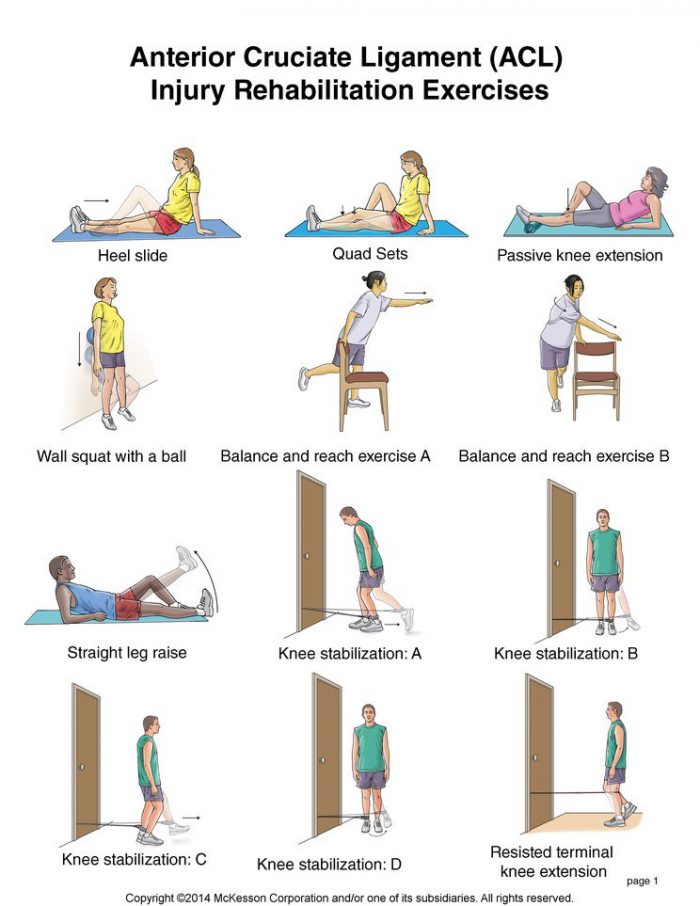
The benefits of leg extensions are their ease of use and isolation. Leg extension machines require little balance and coordination since the movement is machine guided and non-weight bearing (seated). Thus, leg extension devices are excellent for beginners or after an injury (rehabilitative) if prepared correctly. Leg extensions enable direct overload of the quadriceps without the involvement of other muscle groups and can help to correct imbalances in muscle development and increase volume in the quadriceps at the end of a workout.
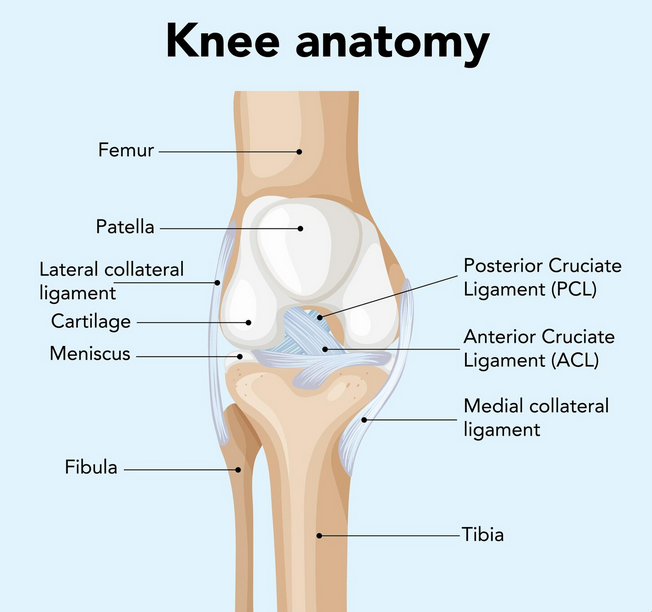
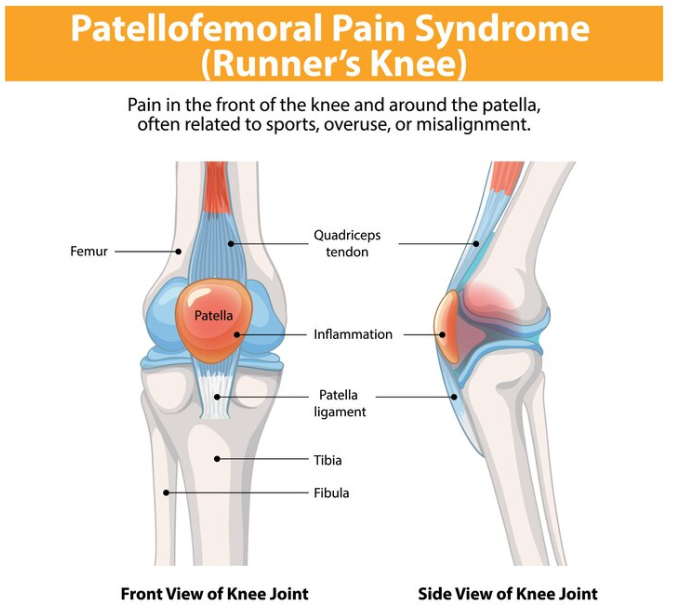
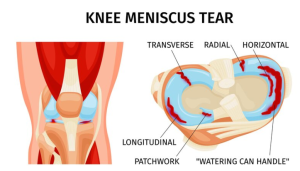
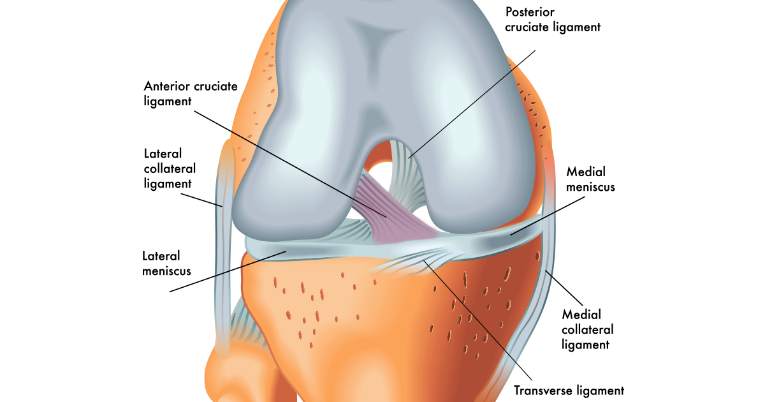
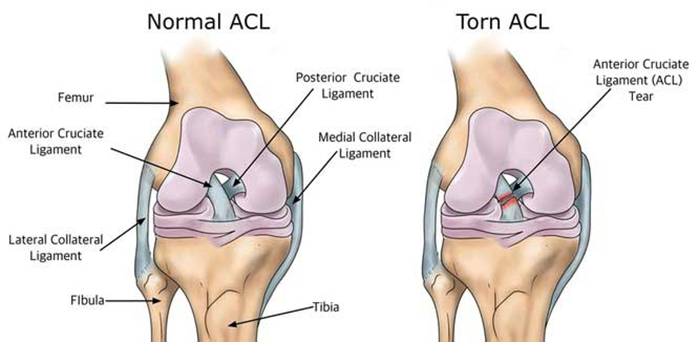
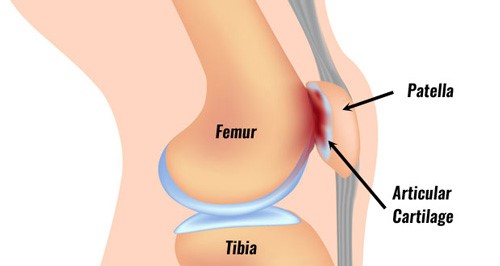
However, due to their isolation nature, leg extensions have a number of limitations. Leg extensions are performed with a seated base and a fixed movement pattern, which do not replicate the natural leg movements we undergo in our daily lives or the leg movements performed in sports. Also, leg extensions place a large amount of stress on the knee joint, mainly when they are performed with heavy weights or with poor technique.
Conversely, squats are considered one of the best lower body exercise options available. They imitate the motions we use each day, like sitting down and standing up, lifting objects from the floor and more. They also help improve joint range of motion especially at the hips, ankles, and knees and developing strength usable throughout life. Additionally, squats recruit multiple muscle groups to perform an activity. This allowss for maximum overall strength development, an increase in muscle mass, and a higher volume of calories burned. As physiotherapists, we refer to squats as functional movements due to their real world carry over and ability to reduce the chance of injuries.
So which one is better?
So now the question arises, which type of exercise will best suit you? Most people who exercise should include squats in their routine as the foundation of their leg workouts. Squats allow the development of overall leg strength as well as improve balance, and when done correctly, squats promote good long-term joint health for those doing a lot of sitting and standing. Although not every person who trains their lower body will be an athlete, having strong legs is an important aspect of staying active and fit. A strong leg foundation is also beneficial to those who are trying to lose fat or improve daily movements, as good leg strength helps create a solid base of stability for any physical activity.
While squats are excellent for developing strength and balance, leg extensions also have a place in a complete lower-body workout program and can be an effective way to work on isolated quadriceps strength, to address a specific weakness and for increasing muscle definition without putting a high demand on the rest of the body.
Instead of trying to choose between squats and leg extensions, the most effective approach is to combine the benefits of each exercise, so everyone benefits from both improving their lower-body strength and developing good muscle definition. Prioritizing squats while supplementing with leg extensions will enable everyone to build strong and functional legs while still having a strong focus on building muscle, thus giving the best overall performance and appearance.
Have more questions?
Look for PhysioNow! We have expert clinicians ready to assist you with any training questions you may have. If you are struggling through any kind of knee pain, leg pain, or even anticipating an upcoming surgery whether it is a total knee replacement or an ACL repair, we will help you through it all! One of the most important parts of training is learning how to stay injury free, so book with PhysioNow today for you first assessment and treatment! Look for us at one of our 10 west GTA locations including Burlington, Oakville, Mississauga, and Etobicoke! P: 289-724-0448 Email: applewood@physionow.ca