Trochanteric bursitis
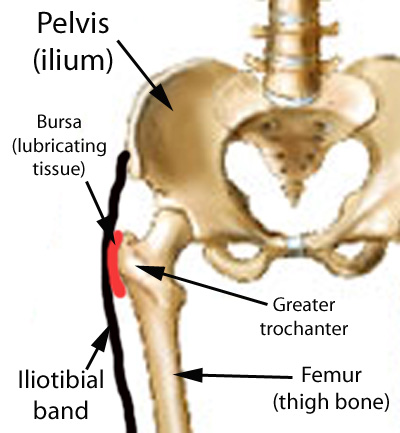
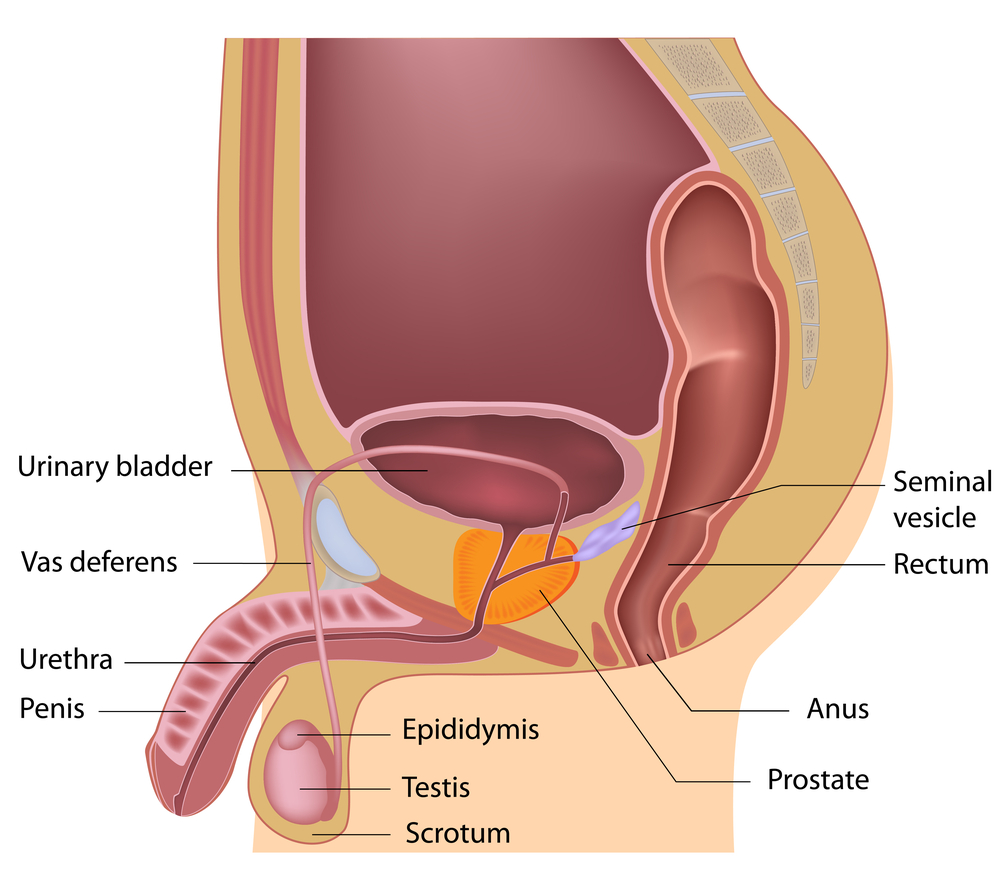
The Trochanteric Bursa is a fluid filled sac near the hip joint. It cushions between the bones and the muscle and acts as a shock absorber. Trochanteric bursitis is the inflammation of the bursa which is at the outside of the hip.
When this bursa is irritated it causes pain on the outside of the hip and thigh. Sometimes you may feel the pain down to the knee on the same side. Another symptom is pain which will stop you from lying on your painful side. It will be painful when you press on a specific spot on the outside of the hip. The pain gets worse when climbing stairs, getting up from a low chair getting out of a car. Sitting with crossed legs hurts. Both walking and running may also cause increased pain.
Causes of Trochanteric Bursitis
- Any direct Injury to the outside of the hip like falling, or bumping into an object.
- Incorrect posture due to muscle imbalance
- Leg length difference.
- Stress of soft tissues surrounding the hip due to hip Osteoarthritis
- Friction of the ITB (Ilio Tibial Band: a muscle along the side of the hip)
- Overuse injuries like standing for long periods of time
- Other diseases which affect the hip like Rheumatoid Arthritis
- Previous surgeries around the hip
- Very rarely infection of the bursa
Registered Physiotherapy Treatment
Your Registered Physiotherapist can help you to reduce the pain and inflammation. They will use electrotherapy modalities, taping, or acupuncture. They will give you advice on activity limitations in the early stages.
Later the treatment is focussed towards increasing the flexibility and strength in the muscles. Your Physiotherapist will increase the hip joint range of movement and correct your hip joint mechanics.



Finally the focus is towards preventing it from happening again.
General Advice on prevention
Your Registered Physiotherapist will look at your posture, hip stability, and core strength. They will look to see if you need Orthotics to address any problems with your legs or feet.
Tips for prevention of Trochanteric Bursitis:
- Whenever you start a new activity, try to take it slow and build up your activity level gradually.
- Start with less force or resistance, less repetitions and progress gradually.
- Avoid or modify repetitive activities if it is putting any stress on the hip joint
- Your footwear should be comfortable
- Maintain flexibility and strength in your lower extremity muscles
- Improve your core muscle strength
If you or someone you know may have Trochanteric bursitis, call PhysioNow Today! We would be happy to get you started on your treatment and back to enjoying all the things you love to do!

 may also be beneficial as a treatment for Golfers elbow.
may also be beneficial as a treatment for Golfers elbow.
 Resolution of the symptoms after surgery can be more temporary if the symptoms originate from elsewhere. Our experienced Registered Physiotherapists at PhysioNow will assess you to find out the actual cause of your symptoms and will help you to get rid of your symptoms. Call
Resolution of the symptoms after surgery can be more temporary if the symptoms originate from elsewhere. Our experienced Registered Physiotherapists at PhysioNow will assess you to find out the actual cause of your symptoms and will help you to get rid of your symptoms. Call 