Fracture types
Fracture Rehabilitation
Fractures are common injuries . They can happen to people of all ages, from the very young to the very old. The majority of fractures occur with trauma to the bone. It could be either from a fall or a blunt force. Most people can readily feel that they have a broken bone. This is because the signs and symptoms can be very obvious.
Some of these indicators of Fracture are:
- Swelling or bruising over a bone
- Deformity of an arm or leg
- Pain that gets worse with any movement or added pressure
- Inability to put any weight through the injured area
- Protruding bone through the skin (in the case of open fractures)
In some cases, however, fractures can be less obvious. Some ankle fractures may look a lot like ankle sprains. You may not even know that it was a fracture until it shows up on an X-ray.
Spine Fractures
Fractures through the spine may feel a lot like back pain initially. This is due to the make-up of the spine. Bony injuries to the back do not produce any of the obvious signs and symptoms . However, one of the key components of a spinal fracture is that it occurs after some sort of trauma. This is most commonly a fall. Therefore, if there is a traumatic event reported, the physiotherapist will rule out any potential spinal fracture. They will do a thorough assessment. If the Physiotherapist suspects a potential fracture, we will refer you back to your doctor to get X-rays done.
Fragility Fractures
In people with osteoporosis, fractures can happen with very minor stumbles or movements. Osteoporosis is a condition where the bones become fragile or brittle from loss of bone. Fractures associated with osteoporosis are called fragility fractures. They occur due to the weakness of the bone itself.
If you have Osteoporosis, your bones can be injured with small traumas that would not normally affect the average person. If you have back pain and you have had trauma, the Physiotherapist will ask whether you have osteoporosis. This is to rule out potential fragility fractures.
Diagnostic tests for a Fracture
In any incident where there is a suspicion of a fracture, X-rays are necessary. This will confirm the presence of the fracture, its exact location and severity. However, in some cases, an X-ray may not be sensitive enough to show the fracture. In these situations, if a fracture is still suspected, more sensitive tests like a CT, MRI or bone scan may need to be completed.
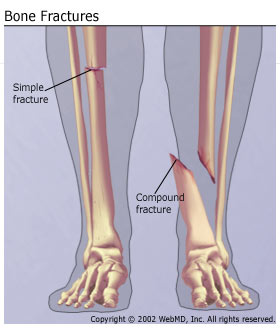
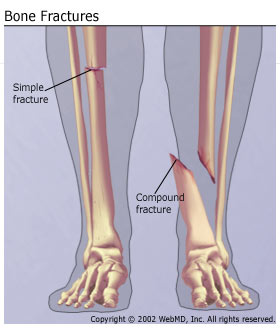
Fracture Classifications
There are 4 main classifications of fractures:
- Displaced – the bone snaps into 2 or more parts and moves so that the two ends are not lined up straight.
- Non-displaced – the bone breaks partly or all the way through, but the ends remain lined up
- Closed – the bone breaks but there is no puncture wound in the skin
- Open –the bone breaks through the skin
Types of Fractures
There are also 7 different types of fractures to describe the specific nature of the break line:
- Greenstick – incomplete fracture, where the broken bone is not completely separated
- Transverse – the break is in a straight line across the bone
- Spiral – the break spirals around the bone, common in a twisting injury
- Oblique – the break is in a diagonal line across the bone
- Compression – the bone is crushed, causing the broken bone to be wider or flatter in appearance
- Comminuted – the break is in three or more pieces
- Segmental – the same bone is fractured in two places, so there is a ‘floating’ segment of bone
Fracture Treatment
In terms of management of fractures, the treatment depends on the type of fracture. The fractured ends of the bone must be set in their proper place and held there for the bone to heal properly. This process is called reduction.
Fracture Repositioning
Most fractures are repositioned without the need for surgery. This is called closed reduction. Once the bones are positioned properly, the joint is casted . The length of casting is usually 6 weeks. This is how long it typically takes the fractured bones to heal. There are circumstances where the period of casting may be either shorter or longer. This depends on the nature of the fracture. If it is an ankle or foot fracture, the doctor may also recommend that you wear an aircast boot to stop your foot from moving.
PhysioNow carries a full supply of these aircast boots if you need one.
Open Reduction (Surgery) after Fracture
Open reduction (surgery) is done for fractures that are more complicated. The repositioning of the bones wil be done with surgery in this case. The surgeon will use screws and or plates to keep the bone fragments in proper position. This allows for proper healing. Following open reduction, you will have a period of immobilization . The length of time for a fracture thathas required surgery will depend on the bone that was fractured. It also depends on the severity of the fracture. Also, depending on the fracture and the needs of the patient, the hardware may either be left in permanently or taken out with another surgery. If removal of the hardware is necessary, it will happen once the fractured bone has completely healed.
Spinal and Rib Fractures
There are however some fractures that cannot be effectively immobilized such as spinal and rib fractures. For these types of fractures, the affected area is protected with avoiding certain activities or postures.
Healing times for Fractures
In terms of healing times, most uncomplicated fractures take approximately 6 weeks for the bones to fuse. Although medically, the fracture would have healed, there may still be a lot of limitations. For fractures that are more complicated and required surgery, the healing times may be a little longer due the surgery.
Delayed Healing of Fractures
There are also some people who will heal at a slower rate because of various health conditions or medication use. So, if you have diabetes, osteoporosis or are a long time user of prednisone, you may fall into this category. Scaphoid Fractures also may have delayed healing because there is a poor blood supply to the bone.
Registered Physiotherapy after Fractures
Once the fracture itself is healed, there may still be some remaining problems from the injury. Since the fracture would have been immobilized for several weeks, there will be a significant loss of movement and strength around the broken bone.
It is important to follow up with Physiotherapy for Fracture Rehabilitaton. This helps to ensure that there can be a safe return to all previous activities. A Registered Physiotherapist will be able to assess the limitations. They will prescribe the necessary range of motion and strengthening exercises and then you can get back to all of your normal activities quickly!
PhysioNow Etobicoke and Mississauga
PhysioNow has highly trained Registered Physiotherapists on staff to help you after a Fracture. We are open evenings and weekends to help meet your needs. We also do direct billing to your insurance plan if you have one and if they allow us to do so on your behalf.
Call today to get started on your Fracture Rehabilitation!