Acute Ankle Sprains
Acute Ankle Sprains
How do Acute Ankle Sprains happen?
Acute Ankle sprains are common injuries in people of all ages. They can happen in many different circumstances. However, they always involve some type of fall or twisting movement to the ankle. For example:
- Going downstairs and missing the last step resulting in twisting the ankle
- Landing on the ankle in a twisted position after coming down from a lay-up in basketball or in a Sports Injury
- Slipping on an icy street while walking
In all of these situations, the ankle gets a sudden movement and/or trauma that causes it to twist more than its normal range of movement allows.

Acute Ankle Sprains
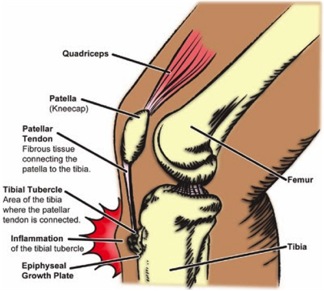
What structure gets injured with an acute ankle sprain?
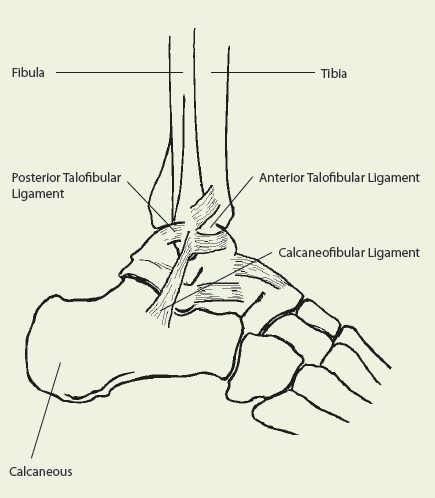
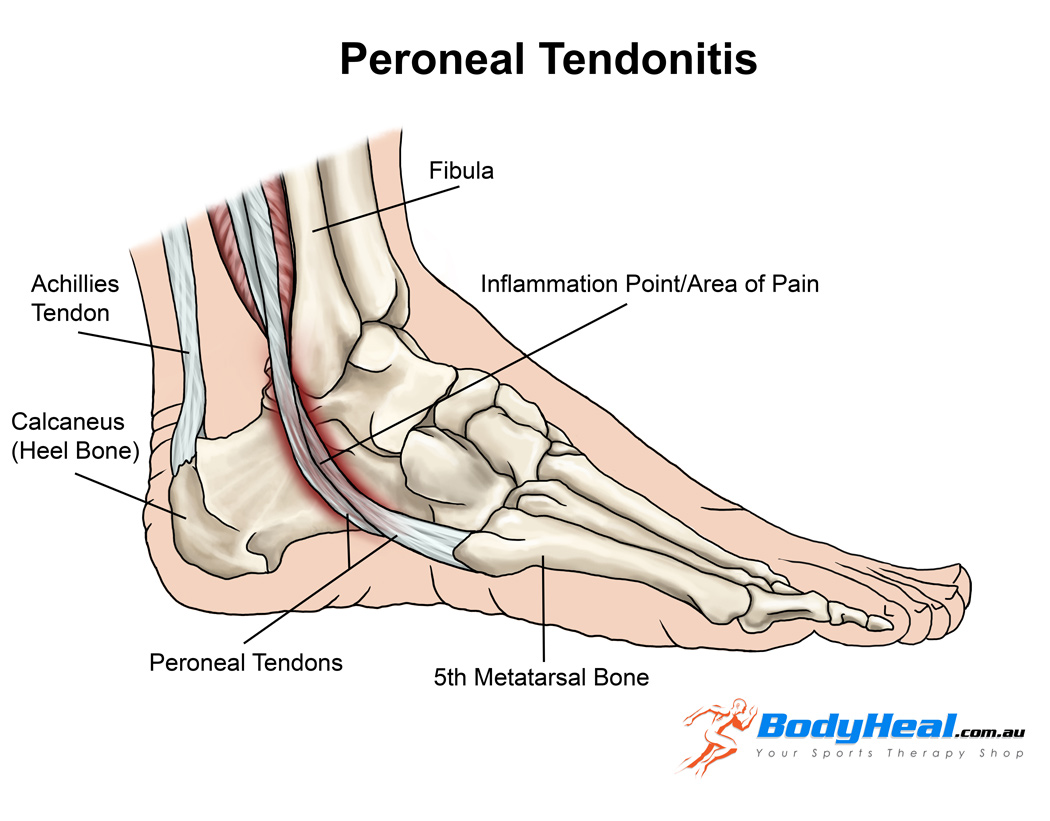
The structures that are injured with acute ankle sprains are the ligaments around the ankle joint. Ligaments are soft tissue structures that connect two bones together. Their function is to prevent the bones from moving too far away from each other. Ligaments help maintain normal movement between the bones.
With ankle sprains, the ligaments get over-stretched beyond what they can tolerate which causes tears in their fibres. The ligaments that are involved in acute ankle sprains are present on the outside (lateral), inside (medial), and top of the ankle.
Are there different types of acute ankle sprains?
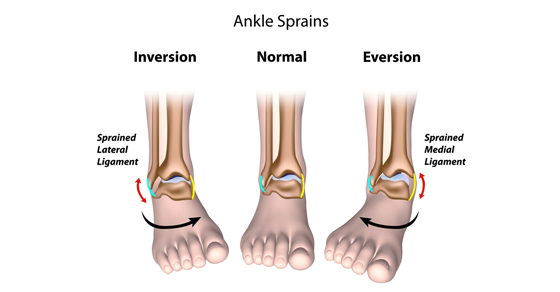
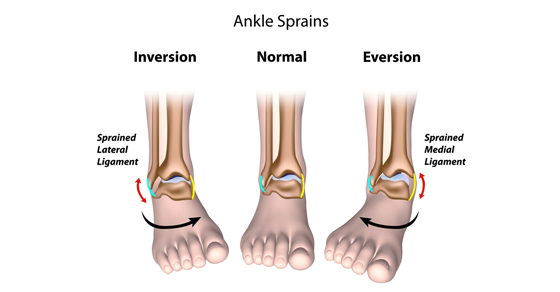
There are three main types of ankle sprains:
- Inversion
- Eversion
- High Ankle Sprain
The terms relate to the direction of ankle movement that caused the injury to occur.
INVERSION ANKLE SPRAIN
- An inversion sprain occurs when the ankle is forcefully turned inwards.
- This type of acute ankle sprain is the most commonly occurring of the three because the ligaments on the outside of the ankle are generally weaker than the rest.
- Another name for an inversion ankle sprain is lateral ankle sprain
- A lateral ankle sprain injures the ligaments on the outside of the ankle.
EVERSION ANKLE SPRAIN
- An eversion sprain occurs when the ankle is forcefully turned outwards.
- This type of force injures the ligaments on the inside of the ankle.
- The ligaments on the inside of the ankle are called the deltoid ligament
- An eversion ankle sprain is also called a medial ankle sprain
HIGH ANKLE SPRAIN
- A high ankle sprain is the rarest of the three types and it occurs when there is excessive twisting of the shin.
- The ligaments that are injured with this type of injury are located above the ankle.
- The location of the ligaments is why this injury is called a ‘high’ ankle sprain.
Are some people more at risk for Acute Ankle Sprains than others?
There are certain risk factors that may make ankle sprains more likely to happen. However, the research is a little inconclusive on why this is so. Some of these possible factors include:
- Poor muscle strength/fitness
- Increased weight
- Decreased muscle-reaction time
- Previous history of ankle sprains resulting in poor balance
Can there be different severities of Acute Ankle Sprains?
The severity of the ankle sprain depends on how much the ligament was overstretched in the process of the injury. Sprains are classified by different grades to explain the severity:
- Grade I: mild stretching or tear of the ligament, with little or no instability at the joint
- Grade II: incomplete tear of the ligament, with some instability in the joint
- A Grade III: ligament is completely torn or ruptured and there is no stability in the ankle
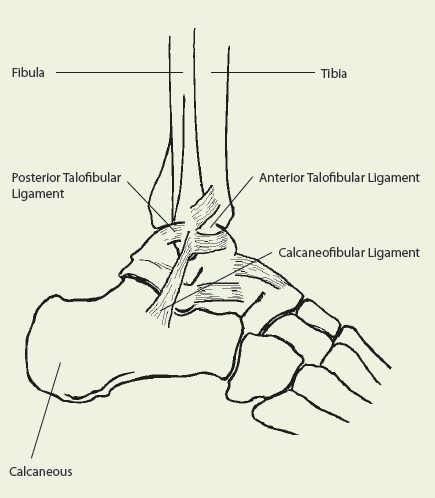
Ligaments affected in Ankle Sprains
What should you do if you think you have sprained your ankle?
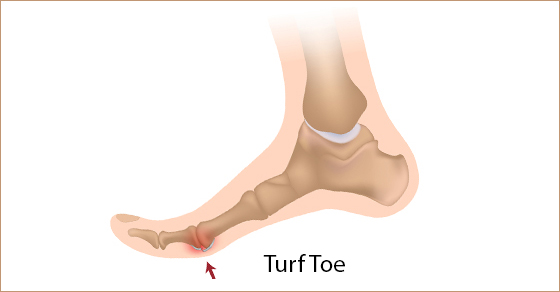
In all three types of Acute Ankle Sprains, it is important that you see a health care provider. The health care provider, whether it is a doctor or a Registered Physiotherapist, will first rule out the possibility of fracture. There is always the possibility of a fracture with Acute Ankle Sprains. The ligaments attach onto a bony area and if the twist is severe enough, it can pull off a chunk of the bone. When this happens, it can cause a fracture. Signs and symptoms of a potential fracture include:
- Lots of swelling
- Increased bruising
- Increased tenderness over specific areas of the ankle
- Difficulty or inability to put weight through the injured ankle
When the signs and symptoms are suspicious of a fracture, then an X-ray must be completed. If there is no evidence of fracture, then your doctor may send you for an ultrasound. In the end, they should refer you for Physiotherapy treatment. So ask your doctor to send you to Physiotherapy if they don’t think to recommend it themselves.
What will happen during my first Physiotherapy appointment?
During the Physiotherapy assessment, your Registered Physiotherapist will assess everything to do with your Acute Ankle injury, including:
- Pain intensity and location
- Swelling
- Sensation
- Range of motion
- Ankle stability
- Strength
- Balance
This will provide some baseline information for your Physiotherapist.
How can Registered Physiotherapy help treat Acute Ankle Sprains?
The treatment for acute ankle sprains depends on the type of sprain as well as the severity of the injury.
Immobilization
- Because of their affect on ankle stability, a Grade II or III injury will require some immobilization. This is usually done through a removable walking cast.
- The purpose of the immobilization is to protect your injured ligaments from movement and external stressors, so that they can heal.
- The period of immobilization will depend on the injury and your health care provider will provide specific instructions.
- A grade I sprain will not require any immobilization because the stability of the ankle is still intact. However, your Physiotherapist will recommend activity modification to help with the healing process.
Physiotherapy Treatment in the acute phase?
- In the initial phase of the treatment, the Physiotherapist may focus on pain relieving modalities
- Electrical modalities like IFC and Ultrasound can help relieve pain and swelling
- The Physiotherapist will also prescribe gentle mobility exercises to help improve or maintain movement through the ankle
- The length of the acute phase depends on the severity of the sprain

Ankle Rotations for movement Recovery
Treatment in the later stages of Acute Ankle Sprains
- Once the ligament healing is underway and the patient feels a little better with their pain, the treatment will get more progressive
- It will focus on regaining mobility, strength and function through the ankle
- Your Physiotherapist will prescribe exercises that are going to help regain the lost range of motion and strength.
- Over several weeks, the exercises will be progressed as you improve.
- Another important aspect of treating an ankle sprain is including balance re-training in the program.
- Balance is very much affected after an ankle sprain and it is something that must be improved with specific exercises. This is very important no matter whether you are returning to Sports or just everyday living! Balance Retraining is key to Falls Prevention!
- We use our balance ability on a regular basis with walking on uneven surfaces or when trying to recover from a stumble. Therefore, it is important to improve balance ability to prevent any possible re-injury of the ankle.
- If you have had an acute ankle sprain before, and DID NOT attend Physiotherapy, it is likely that you are at increased risk of reinjuring your ankle or falling again!

Physiotherapy Mobilizations
Do I need to get Physiotherapy treatment after Acute Ankle Sprains?
There are some people who have sprained their ankle multiple times and never sought out treatment for the injury. They usually give themselves some time for the pain to get better and then go about their usual activities.
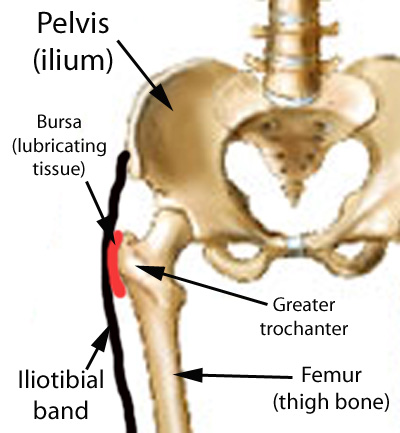
This type of management is not usually recommended because multiple ankle sprains can affect the stability of your ankle. As a result, this may create problems in the future. Also, the reduced stability in your ankle may cause compensations in your knees and hips. This can complicate the picture and make your injury more complex.
It is therefore recommended that you seek out proper Registered Physiotherapy care to address an ankle sprain soon after it occurs. This ensures that your acute ankle sprain heals in a timely manner without added complications. The most important part of treatment is regaining your balance. If you do not do this, another injury in quite likely.
To get started on your Acute Ankle Sprain Treatment, Give PhysioNow a call Today!