Accident Rehabilitation
What is Accident Rehabilitation?
Motor vehicle accidents happen everyday in Ontario. As a result, they produce a lot of pain, disability and stress for those involved. The impact can be quite debilitating. Accident rehabilitation is treatment that is given after being involved in a motor vehicle accident. It is important to seek out Registered Physiotherapists who are experienced in Accident Rehabilitation to ensure proper recovery. At PhysioNow we offer high quality Registered Physiotherapy and Registered Massage therapy treatments to help you recover from your injuries.

Registered Massage Therapy
Who is entitled to receive Accident Rehabilitation?
Any person who has been involved in a motor vehicle accident in Ontario is entitled to receive Accident Rehabilitation benefits . This would include if you were a pedestrian hit by a vehicle. It would also include coverage for treatment if you were involved in an accident outside of Ontario, but reside in Ontario. However, if you are injured and do not have your own insurance, you can still apply for accident benefits. The circumstances of the accident will determine which insurance company will pay for the benefits. For instance, you may be covered by the person that hit you or the Motor Vehicle Accident Fund.
How much accident benefit coverage is available?
The amount of the benefits that you are entitled to depends on the severity of your injuries. There are two categories of benefits available:
-
Minor Injury Guideline (MIG)
- This plan is for people who have minor injuries including whiplash and sprains and strains.
- The majority of motor vehicle accident injuries fall within this category
- The MIG plan is standardized across all of Ontario in terms of its entitlement to Treatment benefits no matter where you receive treatment.
- If you are under a MIG, the maximum benefit under the MIG is $3500
-
Major Injury Guideline (non-MIG)
- This plan is for people who have suffered serious injuries from an accident
- Examples include fractures, surgeries, major neurological trauma and concussions
- The maximum entitlement under this plan will vary depending on your injuries, but could be up to $65,000.
What is the process of receiving accident benefits?
Once the accident is reported to the insurance company, the adjuster will ask if there are any injuries from the accident. The adjuster will send you a package of forms that you have to complete and send back. The adjuster will also likely put you in touch with an approved physiotherapy clinic in the area closest to you. The clinic will then contact you to schedule an initial assessment.
1st visits with a Physiotherapist can take place within 1 day of the accident. You are also able to go directly to your Approved Physiotherapy Clinic to initiate a claim and get started on your treatment. The Approved Clinic can get the paperwork started for you.
PhysioNow is an approved company for the purposes of Motor vehicle accidents in Ontario. PhysioNow is allowed to directly bill your treatment to your Auto Insurance company. They can provide all of the forms that you need to get started.

Whiplash Pain
What are the most common injuries from a Motor Vehicle Accident?
Most car accidents tend to be minor in nature. The most common types of injuries are:
-
Whiplash
- Happens when the force of the impact pushes your neck back and forth really fast
- This causes a sprain/strain of the your muscles and ligaments of the neck
- Symptoms range from pain, stiffness, numbness/tingling into the arms and hands, headache and loss of motion
-
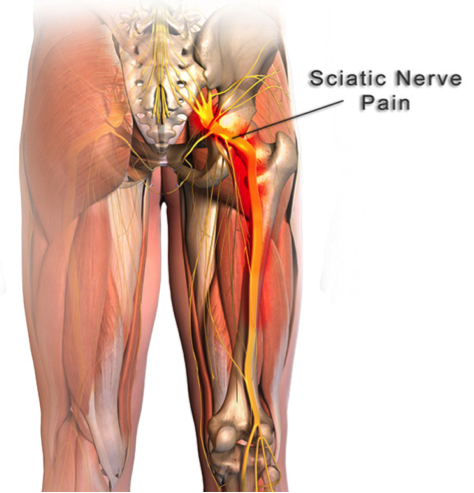
Thoracic & Lumbar strains
- The impact causes the joints and muscles of the spine to be over-stretched
- The mechanism is similar to whiplash
- Symptoms include pain, limited movement, numbness/tingling into the arms and/or legs, weakness
-
Shoulder strains
- It is common for the shoulder to get injured in a car accident, especially for the driver – this is because their arms are usually holding on to the steering wheel
-
Concussion
- Concussions are a form of a traumatic brain injury and can vary from mild to severe
- It is possible for Concussions to occur as a result of either direct or indirect trauma to the brain
- The most common symptoms of a concussion are dizziness, nausea, sensitivity to light and sound, headache, fatigue, difficulty concentrating and fogginess
-

Concussion
What can I expect from my first visit at the physiotherapy appointment?
During the initial visit, you will have to complete some forms. These forms are essential to submitting a successful claim. The experienced administrators at PhysioNow can help you to fill them out to make the process easier for you. The good thing about the paperwork is that you only need to complete it once! After the initial paperwork, you can focus just on your recovery.
What can I expect from my Initial Assessment with the Registered Physiotherapist at PhysioNow?
Your Registered Physiotherapist will meet with you. We will start by asking some questions to get an understanding of your injuries. For example, some sample questions can include:
- How did the accident happen?
- Questions that will screen you for more serious injuries that could require further medical attention
- Locating all the painful areas and injuries that have occurred
- Details about past medical and injury history
Once this information has been collected, your Registered Physiotherapist will do a full assessment. We will check all of your affected areas for movement and strength. This will start to give us an idea of the severity of your symptoms. We will then use this information to decide whether you will be classified as either MIG or non-MIG.
After this, we will then fill out the required treatment plan for you. In conclusion, we will go over what the plan will look like with you. Lastly, they will discuss treatment timelines and treatment goals. At PhysioNow, there will also be time allocated to start some light treatment to give you pain relief.
What kind of treatment will be provided for Accident Rehabilitation?
The types of treatment provided after vehicle accidents will depend on the nature of your injuries. It will also depend on what your Physiotherapist feels is most appropriate for you, taking into account all of your injuries. As a result, your treatment plan may include a variety of different treatments such as:
- Treatment will start slowly at first and focus first on pain control,
- Modalities – Ultrasound, Laser, Interferential Current
- TherapyManual therapy – gentle soft tissue work, mobilizations, assisted stretching
- Exercises – range of motion, postural and strengthening exercises
- Concussion Treatment if needed
- Education – explanations of the injuries and do’s and don’ts to help the recovery process
- After that, this will be followed by recovery of movement, and then strength.
- Lastly, we will work on helping you get back to all of your normal activities both at home and work
-

Accident Rehabilitation
How long will the treatment take to complete for Accident Rehabiliation?
The length of the treatment plan depends on whether you are on a MIG or non-MIG pathway.
- MIG (Minor Injury Guidleline)
- 2 phases
- 1st phase: 12 weeks in length
- 2nd phase (if required): additional 4-8 weeks
- Non-MIG ( Non- Minor Injury Guideline)
- Timeline is at the discretion of your physiotherapist and will vary depending on your injuries
- For post-surgical cases or individuals with multiple serious injuries, the timeline can be well over 1 year
- 2 phases
As a result, it is very important to seek out Accident Rehabilitation as soon as possible when you have been involved in a car accident. The pain and limitations that you experience after an accident can really affect your quality of life. Therefore, scar tissue from injuries starts to form quickly after an injury.
At PhysioNow we want to help you get back on your feet and back to doing things that are important to you! Give us a call at 289-724-0448 to get started today!





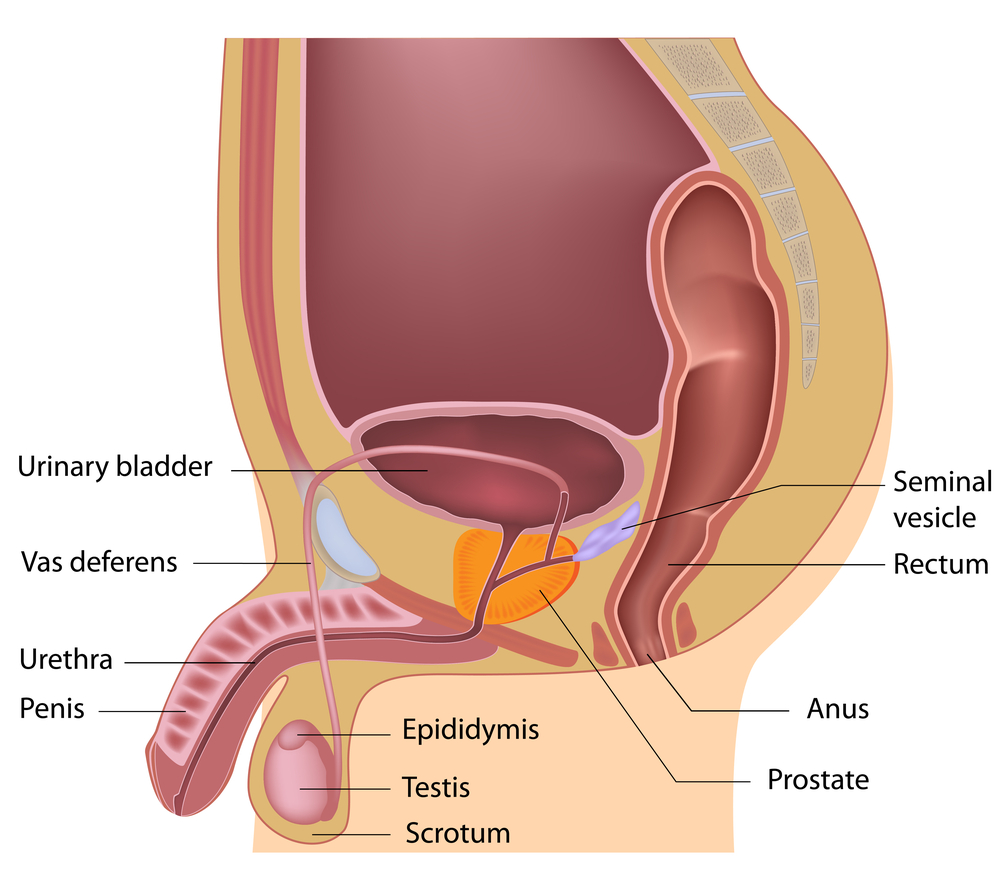
 Female & Male pelvic pain
Female & Male pelvic pain