Trigger finger? What to do
Lately you’ve noticed that your finger seems to be clicking, and maybe it also catches or locks into a bent position. Sometimes you may need to use your other hand to help you “unlock” your finger. What is this? We call this condition trigger finger.
Your finger locks in a flexed position. The position it locks in resembles the position of a finger when it is pulling a trigger.
If you have trigger finger, you may also have:
- Stiffness and swelling, especially in the mornings.
- Painful or painless clicking, catching, locking into the bent position then popping straight.
- Loss of full range of motion of the fingers into flexion and extension (bent and straight).
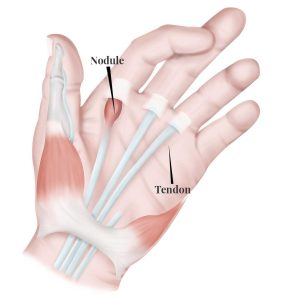
- Nodule is felt with other hand.
- Pain that radiates to the tip of the finger and/or into the palm.
Why does Trigger Finger happen?
An exact cause is unknown, it develops spontaneously or consequently to another disease, repetitive hand movements during a job, or recent trauma to the hand.
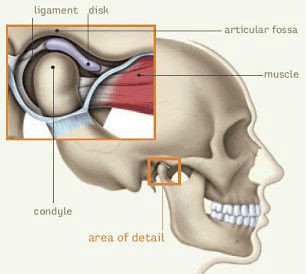
The condition occurs due to inflammation and narrowing in the “pulley” system in the hand. As seen in the image below, the tendons of our muscles must pass through a band of tissue in order to control the fingers. The tendon normally glides through this tunnel without issue but the tissue of the tunnel can thicken and narrow, combined with enlargement of or nodules developing in the tendon itself, resulting in impaired movement and the tissues blocking each other.
How to treat trigger finger?
The first line of recommended treatment for any condition is conservative care. A physiotherapist can help you recover your hand function and quality of movement. These treatments
may include:
- Soft tissue techniques, joint mobilizations, and stretches to try and increase the mobility in the
area. - Modalities like ice, paraffin wax, and electrical stimulation to help with pain, inflammation, and swelling.
- A home exercise program that focuses on increasing range of motion, strength, and gliding of the tendons
- Education on wearing a splint (as shown below) which blocks the finger from moving excessively, allowing you to go about your daily life without aggravating the condition. Wear this between 6-10 weeks and your physiotherapist may ask you to wear them at night, during work, or as much as possible during the day.
What options do you have for treatment?
In some cases, this condition may be persistent and medical management with your primary provider. For example, options
may include corticosteroid injections to reduce inflammation and the frequency of the finger locking. Unfortunately, patients may require further intervention when conservative treatment fails, in which case a surgical release of the finger may be indicated. When combined with physical therapy after the surgery, there is usually a rapid and significant improvement in function at relatively low risk. However, there are always increased risks to surgical procedures compared to conservative treatment and where possible, trigger finger should always be treated with non-surgical strategies first and surgery as last resort.
Need some help?
Let us manage your trigger finger. Here at PhysioNow, we have many highly knowledgeable physiotherapists that can assist you with your issue. If you think you have trigger finger or have been diagnosed with it, book with PhysioNow today for your first assessment and treatment!